Summary
DOI: 10.1373/clinchem.2013.210534
A 79-year-old white man with a history of progressive bone pain was admitted for evaluation 3 years ago. The patient reported that the pain began in both feet and gradually spread to the rest of the body over a 2-year period. Further assessment revealed multiple stress fractures in the feet.
Student Discussion
Student Discussion Document (pdf)
Qing H. Meng1* and Elizabeth A. Wagar1
1Department of Laboratory Medicine, The University of Texas MD Anderson Cancer Center, Houston, TX.
* Address correspondence to this author at: Department of Laboratory Medicine, The University of Texas MD Anderson Cancer Center, 1515 Holcombe Blvd, Unit 37,Houston, TX 77030-4009. Fax 713-792-4793; E-mail: [email protected].
Case Description
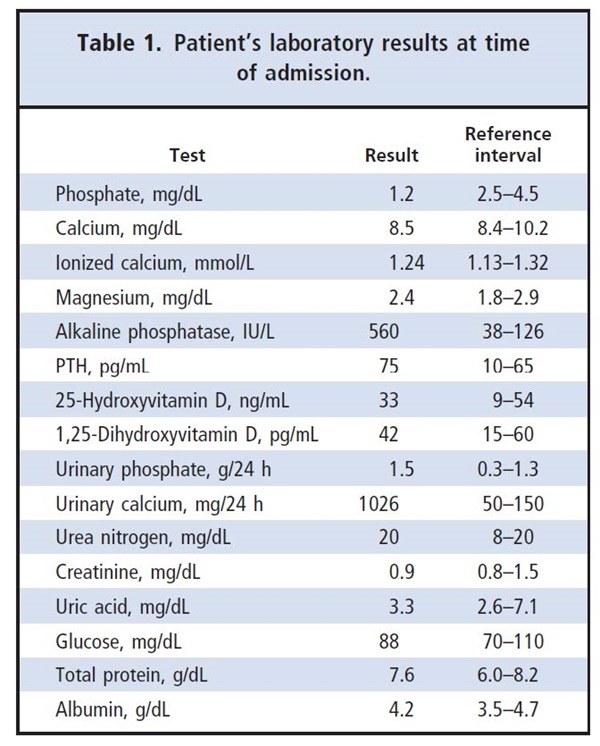
A 79-year-old white man with a history of progressive bone pain was admitted for evaluation 3 years ago. The patient reported that the pain began in both feet and gradually spread to the rest of the body over a 2-year period. Further assessment revealed multiple stress fractures in the feet. Bone mineral density test indicated osteopenia. Serial bone mineral density tests during the 2 years showed that his osteopenia was progressing.Results of several serum protein electrophoreses were essentially normal. His medical history,which included surgical removal of a cerebral aneurysm near the sella turcica and bacterial meningitis,suggested no pertinent etiologic factors. Physical examination revealed no clinically significant findings except unsteady gait. His serum phosphate concentrations declined from 2.5 to 1.8 mg/dL over the 2 years before admission. Laboratory test results at the time of admission are summarized in Table 1. The patient’s phosphate concentration reached a nadir of 1.2 mg/dLat admission.
His serum alkaline phosphatase was increased.Other notable abnormalities included low normal calcium, normal to borderline high parathyroid hormone (PTH),2 and increased 24-h urine phosphate and calcium excretion. Other routine biochemical parameters [including ionized calcium,thyroid-stimulating hormone, and free thyroxine (T4)] were normal. The patient underwent a whole-body scan showing multiple bone lesions. Diagnostic imaging studies including x-ray, a computer axial tomography(CAT), and MRI of the lungs, abdomen, and pelvis were reported to be normal at admission.Based on the above findings, the patient was diagnosed with osteomalacia secondary to hypophosphatemia. He was then treated with several medications, including bisphosphonates, calcitriol, vitamin D,and calcium and phosphorus supplements. Vitamin Dwas given because his initial calcium and phosphate concentrations were low, and it was discontinued later following improvement of serum calcium concentrations. Despite substantial phosphorus replacement (250 mg phosphorus per tablet, 2 tablets 3 times a day), the hypophosphatemia continued,along with bone fragility and muscle weakness over the next 3 years, and his height decreased from 173 to 163 cm.
Questions to Consider
- What are the common causes of chronic hypophosphatemia?
- What are the possible explanations for hypophosphatemia with hyperparathyroidism and relatively low calcium but normal vitamin D concentrations?
- Which laboratory tests are useful in the evaluation of hypophosphatemia and specifically for the diagnosis of this case?
Final Publication and Comments
The final published version with discussion and comments from the experts appears
in the July 2014 issue of Clinical Chemistry, approximately 3-4 weeks after the Student Discussion is posted.
Educational Centers
If you are associated with an educational center and would like to receive the cases and
questions 3-4 weeks in advance of publication, please email [email protected].
AACC is pleased to allow free reproduction and distribution of this Clinical Case
Study for personal or classroom discussion use. When photocopying, please make sure
the DOI and copyright notice appear on each copy.
DOI: 10.1373/clinchem.2013.210534
Copyright © 2014 American Association for Clinical Chemistry