Summary
DOI: 10.1373/clinchem.2013.207753
A 70-year-old man with a history of hypertension, porcine aortic valve replacement, and chronic obstructive pulmonary disease began having dizziness and confusion. He had strange 1-word responses to his son, who took him to a hospital. A computed tomography scan was performed, showing a subarachnoid hemorrhage.
Student Discussion
Student Discussion Document (pdf)
Irene Shu1 and Ping Wang1*
1Department of Pathology and Genomic Medicine, Houston Methodist Hospital, Houston TX.
*Address correspondence to this author at: 6565 Fannin St., MS205, Houston TX 77030. Fax:713-441-1565; E-mail:[email protected].
Case Description
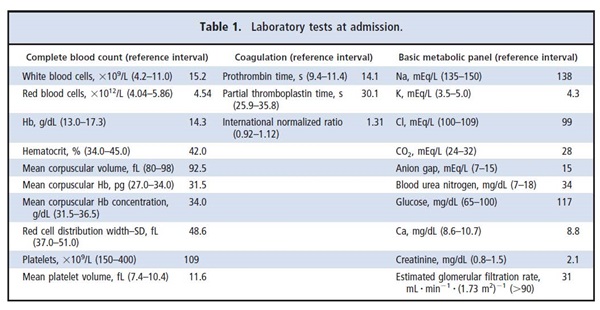
A 70-year-old man with a history of hypertension, porcine aortic valve replacement, and chronic obstructive pulmonary disease began having dizziness and confusion.He had strange 1-word responses to his son, who took him to a hospital. A computed tomography scan was performed, showing a subarachnoid hemorrhage.There was no neurosurgeon at that hospital; therefore,the patient was transferred the next morning to our institution. The patient’s son reported a remote history of falling and the patient hitting his head on a cabinet. The patient denied any headaches, nausea, vomiting,vision changes, or seizures, but he confirmed having a productive cough for the last 2 weeks for which he had been placed on levofloxacin. He smoked 1.5–2 packs of cigarettes a day. His physical examination showed no abnormal neurologic signs, and he was alert and oriented without acute distress. Laboratory tests revealed an increased white blood cell count, abnormal coagulation,and acute renal failure (Table 1). The patient received care and various medications (amiodarone, atorvastatin, azithromycin, benzocaine, citalopram,clonazepam, fluticasone, levalbuterol, metoprolol, andropinirole) at admission to control his blood pressure,cough, throat pain, and subarachnoid hemorrhage.
Two days later (day 3), he developed fever(103.7 °F/39.8 °C) and atrial fibrillation, appeared very lethargic, and complained of mild shortness of breath,but he denied any chest pain, nausea, vomiting, orchills. His renal function had improved. His blood culture from the day of admission was positive for gram-positive cocci, and the physician was concerned for possible endocarditis. The patient was thus given vancomycin and cefepime, and he was scheduled for a transesophageal echocardiography (TEE) procedure the next morning (day 4).
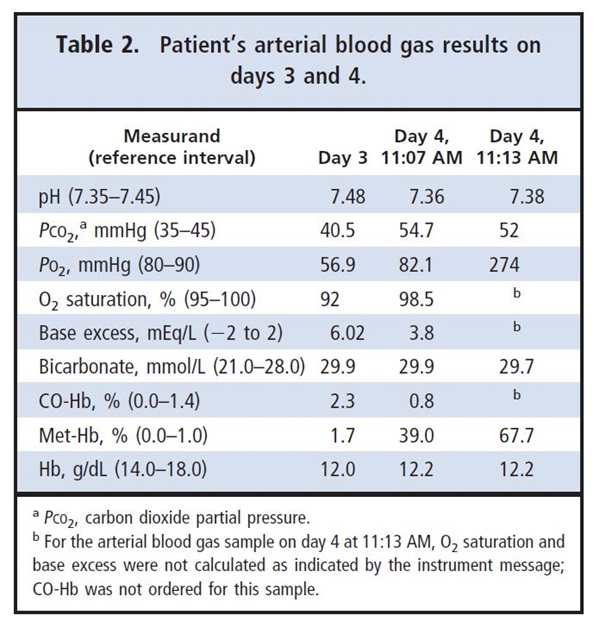
The patient was treated with topical benzocaine spray before the TEE procedure. At the completion ofTEE, the patient experienced respiratory failure, hypotension(87/48 mmHg), and decreased heart rate (57 beats/min), and he was noted to have a cyanotic appearance.The patient was awake and neurologically conversant, and he was able to follow commands. Arterial blood gas changes from day 3 to the morning of day 4 (2 draws that were 6 min apart) are shown in Table 2. Two heparin-containing syringe blood sample son day 4 had a dark-brown color, which was consistent with increased methemoglobin (Met-Hb) levels at 39.0% and 67.7% (reference interval, 0.0%–1.0%).The patient’s pulse oximeter showed oxygen saturation at 77%. The patient’s chest x-ray showed moderately enlarged heart size, atherosclerotic aorta, and minimal pulmonary vascular congestion, with no focal infiltrates or effusions.
Questions to Consider
- What clinical signs and laboratory results lead to a diagnosis of methemoglobinemia?
- What can cause methemoglobinemia, and what was the cause for this patient?
- What methods are available to measure Met-Hb?
- How should patients with methemoglobinemia be treated?
Final Publication and Comments
The final published version with discussion and comments from the experts appears
in the April 2014 issue of Clinical Chemistry, approximately 3-4 weeks after the Student Discussion is posted.
Educational Centers
If you are associated with an educational center and would like to receive the cases and
questions 3-4 weeks in advance of publication, please email [email protected].
AACC is pleased to allow free reproduction and distribution of this Clinical Case
Study for personal or classroom discussion use. When photocopying, please make sure
the DOI and copyright notice appear on each copy.
DOI: 10.1373/clinchem.2013.207753
Copyright © 2014 American Association for Clinical Chemistry