Summary
DOI: 10.1373/clinchem.2011.167213
A 26-year-old woman with end-stage lung disease secondary to cystic fibrosis, cirrhosis secondary to hepatitis C, and insulin-dependent diabetes mellitus presented with acute pneumonia. She was treated with intravenous piperacillin/tazobactam and tobramycin. Other medications included dexamethasone, bumetanide, pantoprazole, dornase, and insulin.
Student Discussion
Student Discussion Document (pdf)
Brian Nagao,1* Shan Yuan,1 and Marjorie Bon Homme2
Divisions of 1Transfusion Medicine and 2Clinical Chemistry, Department of Pathology and Laboratory Medicine, Ronald Reagan UCLA Medical Center, Los Angeles, CA.
*Address correspondence to this author at: Department of Pathology and Laboratory Medicine, Ronald Reagan UCLA Medical Center, 13–145 CHS, 10833 Le Conte Ave., Los Angeles, CA 90095. Fax 310-267-2058;
E-mail [email protected].
Case Description
A 26-year-old woman with end-stage lung disease secondary to cystic fibrosis, cirrhosis secondary to hepatitis C, and insulin-dependent diabetes mellitus presented with acute pneumonia. She was treated with intravenous piperacillin/tazobactam and tobramycin.
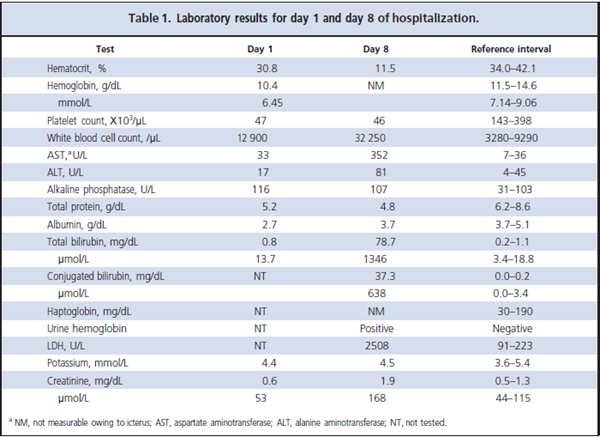
Other medications included dexamethasone, bumetanide, pantoprazole, dornase, and insulin. At admission, the patient’s hematocrit was 30.8% (Table 1). On day 8 of hospitalization, she developed severe anemia with a hematocrit of 11.5%. Her blood type was group A, Rh D-positive, and the results of her antibody screen (performed in solid-phase, low-ionic-strength solution), which had previously been positive for only anti-E antibody, were now positive with a panreactive pattern. The result of the direct antiglobulin test (DAT)3 was 2 + (moderately positive) for IgG, and the eluate was nonreactive. Six units of red blood cells (RBCs) were requested for transfusion. Her plasma was weakly to moderately cross-match incompatible with all group A–positive, E antigen–negative units tested. Given the severity of her anemia, 6 of these units were
emergently released for transfusion to stabilize the patient while the investigation of her anemia and the new serologic findings continued.
Questions to Consider
- What tests are used to diagnose hemolytic anemia?
- What laboratory test suggests the hemolytic anemia in this patient is immune mediated?
- What is unusual about a panreactive pattern on the antibody screen with a negative eluate result?
- How does cirrhosis of the liver affect the laboratory evaluation of hemolysis?
Final Publication and Comments
The final published version with discussion and comments from the experts appears
in the September 2012 issue of Clinical Chemistry, approximately 3-4 weeks after the Student Discussion is posted.
Educational Centers
If you are associated with an educational center and would like to receive the cases and
questions 3-4 weeks in advance of publication, please email [email protected].
AACC is pleased to allow free reproduction and distribution of this Clinical Case
Study for personal or classroom discussion use. When photocopying, please make sure
the DOI and copyright notice appear on each copy.
DOI: 10.1373/clinchem.2011.167213
Copyright © 2012 American Association for Clinical Chemistry