Sometimes seemingly the simplest change can lead to significant improvements in patient care. Such is the case with the winners of the 2021 UNIVANTS of Healthcare Excellence Awards, reinforcing that healthcare improvements don’t necessarily have to be overly complicated to create meaningful and impactful results. From changing the time patient specimens are collected to implementing opt-out screening for HIV to flagging patients at risk for heart failure, these top-ranked integrated clinical care initiatives share one thing in common that is perhaps the most difficult to achieve: Simplicity.
Another commonality that these three winning initiatives share is that they all rely on insights from high quality clinical laboratory testing to improve patient care. Laboratorians were intimately involved on the interdisciplinary teams, developing process improvements that have been recognized by UNIVANTS. The UNIVANTS of Healthcare Excellence award program are prestigious global honors created by Abbott in partnership with AACC and other leading healthcare organizations. The awards recognize teams that collaborate across disciplines to transform healthcare delivery, and ultimately, patient lives. Below we explore the unique achievements of the top winning teams recognized in 2021 as UNIVANTS of Healthcare Excellence winners.
Improving Timeliness of Laboratory Test Results
The COVID-19 pandemic has not only affected patient acuity and case load in the acute care setting, but it also has sparked a movement referred to as “The Great Resignation.”
Combined, these two factors have had a negative impact on patient care. Across the globe, clinical laboratories have seen a significant increase in test volumes while staffing challenges have worsened.
In early October, nursing departments at Banner Health and Laboratory Sciences experienced challenges with balancing the demands of a community COVID-19 surge with nursing and laboratory staffing shortages. They quickly realized that morning routine laboratory tests were increasingly re-ordered as STAT or Timed Study to escalate priority. A re-direction of resource utilization was necessary for the phlebotomy services of the clinical laboratory to keep up with the high demand during the pandemic crisis. Additionally, a house-wide communication plan for resolving day-to-day challenges was needed to help nursing teams, ensuring that patient results were reported for morning rounds, explained Kimm Wuestenberg, MHI, MLS(ASCP)cm, LBBP, CPHQ, associate director, quality improvement at Banner.
“This happened in early October, and I had just attended a National Association for Healthcare Quality seminar that focused on the laboratory’s involvement in quality improvement,” she said. “I happen to be a laboratorian and ended up in hospital quality, so the two fit together nicely.”
For this situation, the team needed a rapid cycle process improvement plan that considered the needs of the laboratory staff, nursing staff, physicians, patients, and payers. A small workgroup comprised of representatives from several different departments – clinical laboratory, medical-surgical, clinical care operations, and quality improvement – formed to work on solutions using an integrated process improvement methodology. They targeted each key stakeholder with the goal of driving change in the short term, while they vetted long-term solutions.
The team chose to optimize an existing process based on the principles of Lean Six Sigma by applying fast and flexible sprint sessions in a small group (Scrum) of department leaders to improve productivity while reducing bottlenecks (Kanban). They also incorporated Design Thinking into the rapid cycle process improvement through innovation with the generation and testing of new ideas. They found that the innovations associated with this project were due not only to the development of an enhanced process, but also in the integration of multiple process improvement methodologies for a successful targeted rapid cycle process improvement project, Wuestenberg explained.
“We changed the specimen collection schedule so that the med/surg results would be ready for morning rounds,” she said. “Instead of collecting specimens in the middle of the night, we had them collected between 10 and 11 the prior evening. Moving it earlier really helped everyone out, and it was great for the patients, too.”
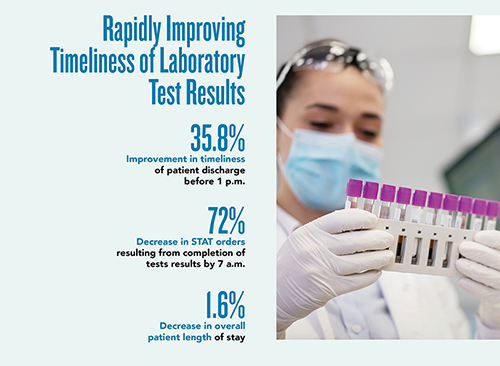
As a result of the process improvement, morning routine laboratory test results were completed by 7 a.m., resulting in early discharges. In fact, discharges before 1 p.m. improved by 35.8%. This is significant because earlier discharge reduces the risk of hospital acquired infections and improves patient satisfaction. The process improvement also led to a 1.6% decrease in overall patient length of stay.
“It seems so simple, but sometimes you just have to go back to basics,” Wuestenberg said. “This helped with the laboratory workflow, it helped the physicians and the nurses, and it was better for the patients.”
Collecting specimens the night before also resulted in a 33% decrease in time studies (TS) and a 72% decrease in STAT orders in the early morning hours. “Earlier test results available to physicians reduced repetitive test orders, specimen collections, and testing duplication,” Wuestenberg said.
As part of the initiative, clinical staff held meetings each day at 3 a.m. to determine if there were any barriers to getting specimens the night before. If there were, nurse leaders ensured that specimens were collected in time for results to be ready for morning rounds. This daily communication between the clinical laboratory and clinical care operations about specimen collection barriers allowed for better resource allocation, according to Wuestenberg.
This initiative, “Utilizing an Innovative Approach to Process Improvement in the Era of a Global Pandemic and The Great Resignation: Rapidly Improving Timeliness of Laboratory Test Results for Multidisciplinary Rounds in an Acute Care Setting,” used various integrative process improvement methodologies, including Six Sigma, Scrum, Kanban, Lean and Design Thinking. The clinical care initiative is highly scalable, Wuestenberg said, noting that this process improvement methodology mix can be used in various circumstances where a temporary solution is needed while leaders work on long-term solutions.
“This is a data-driven process improvement project with laboratory test result timing as the primary focus,” she explained. “This affects physician decision making, patient continuum of care, operations utilization, and payer reimbursement.”
Timothy Hersom, MBA, MT(ASCP), the administrative director of the clinical laboratory, concurred. “The phlebotomy labor shortage and increased number of draws have stretched this finite resource to its limits,” he said. “From the lab’s perspective, the change has given the phlebotomists an opportunity to complete med/surg routine draws first, ensuring that these results are available by 6 a.m. This has a positive domino effect on the turnaround times of lab draws on other units.”
Getting to Zero AIDS
In the United Kingdom, 1 in 14 people living with HIV are unaware of their diagnosis. Croydon, a large town in South London, has an extremely high HIV prevalence area (more than 5 infected per 1,000 people), with more than 46% of those infected diagnosed late in the disease.
In Croyden, 65% of HIV patients are Black African, 50% are female, and 75% are heterosexual, all groups who tend to be diagnosed late.
The marker of late HIV diagnosis is a CD4 count of less than 350 cells/mm3. Individuals with a late diagnosis are estimated to have been unaware of their infection for at least 3-5 years, increasing the likelihood of ill health, premature death, and onward transmission. Early diagnosis allows initiation of highly effective treatment.
Prior to 2020, many emergency departments (EDs) used opt-in testing for HIV, but it was difficult because doctors were uncomfortable asking patients if they wanted to be tested, and most patients do not believe themselves to be at risk or need testing.
In 2020, the British HIV Association (BHIVA) recommended that opt-out HIV testing be implemented in EDs across the UK as a means of diagnosing HIV infection earlier and reducing mortality. In May 2020, a multi-disciplinary team at Croydon University Hospital implemented opt-out HIV testing in its ED. Since implementation of the initiative, at least 97% of all ED patients who had a blood test have been screened for HIV, and the number of new HIV diagnoses has tripled, said Ian Cormack, MD, clinical lead for HIV medicine in the hospital’s HIV Heath Clinic.
Posters in the ED explain that HIV screening will be done automatically unless a patient opts out. If a screening test comes back positive, the patient will be brought back to the hospital for additional testing and will be linked to the appropriate care and treatment.
“This has allowed us to pick up on people with HIV early in the disease progression, before they become ill,” Cormack explained. “HIV can easily be mistaken for many other diseases. It can present itself in so many different ways.”
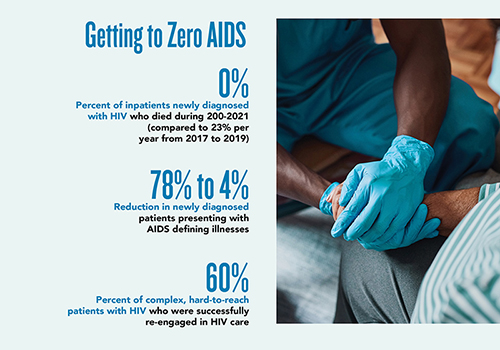
Prior to implementation of the HIV screening initiative, patients typically were tested only if they were already ill, with a significant number ending up in intensive care and/or dying. Since implementation of the HIV screening initiative in May 2020, more than 80,000 people have been screened. Mortality among inpatients who were newly diagnosed with HIV dropped from 23% per year in 2017- 2019 to 0% in 2020-2021. AIDS-defining illness (ADI), which occurs when patients’ immune systems can no longer protect them from life-threatening infections and cancer, decreased from 78% (2005-2010) and 46% (2017-2019) to 4% (2020-2021).
The rate of ADI in newly diagnosed hospitalized HIV patients is now 4%, with 0% mortality and 0% intensive care admissions. The readmission rate in these patients has dropped from 31% (2005-2010) to 0% (2020-2021).
In addition, the average length of inpatient stay has dropped from 35 days (2017-2019) to only 2.4 days (202-2021), thereby freeing up valuable NHS resources during the COVID-19 pandemic. In one year, there were 815 fewer inpatient hospital days for 25 new HIV inpatient admissions, which at £400 per day equates to £326,000. A reduction in readmission rates resulted in additional cost savings of £75,000 per year.
“HIV is straightforward to treat with antiretroviral medication, but patients with unrecognized or undiagnosed HIV can present with dangerous and complex AIDS defining illness,” Cormack said. “These usually have a high mortality rate and carry a significant risk of permanent disability. Starting the correct treatment of these opportunistic infections promptly and ideally within 48 hours dramatically improves outcomes.”
Detecting HIV infection early in someone’s hospital admission dramatically reduces clinical risk and inappropriate investigations or procedures, Cormack added, noting that HIV can affect any body system and can be easily missed or mistaken for another disorder. “For example, people with advanced HIV infection will commonly have weight loss and diarrhea,” he explained. “Without effective HIV testing, they are often referred for colonoscopy and bowel biopsy, which is not necessary. We have witnessed unnecessary colonoscopies being cancelled at our gastroenterology unit as a result of our testing program as the patient’s symptoms got better on starting HIV treatment.”
As a result of the testing program, staff in the HIV health clinic receives a daily list of all HIV-positive patients in the hospital. This allows the HIV team to be involved with their care whatever the reason for their admission. This has improved the quality of their care by allowing healthcare staff to spot any potential drug-drug interactions with anti-retroviral medication (ARV) and any new treatment that has been prescribed, Cormack said, noting that such a negative drug interaction has been prevented at least once a week since the initiative began.
This reduction in ADI presentations has led to a dramatic reduction in hospitalization and HIV deaths, and more than 20 HIV transmissions have been prevented, saving the National Health Service more than £7 million in avoided lifetime healthcare costs. All partners of newly diagnosed patients have remained HIV negative using post and pre-exposure prophylaxis, reducing transmissions to zero. Opt-out HIV testing is now performed in all EDs in extremely high prevalence areas in the UK, and Cormack believes it has the potential to finally get to zero AIDS.
“We did this without any additional resources,” Cormack said. “After two years we finally have some additional resources to make it sustainable and to expand in some other areas as well,” such as primary care physician offices or other medical departments.
An added benefit of the HIV screening is a re-engagement rate of more than 60% of people previously diagnosed with HIV who had stopped receiving care. Prompt, correct management of HIV-related conditions and re-engagement with an HIV service has led to a decrease in mortality among this population from 25% to 16% per year.
“These patients have always had the worst prognosis, as they have a high level of mental health problems, alcohol and substance addiction, and a reluctance or inability to engage with HIV services,” Cormack said. “They often present severely unwell with a high rate of sepsis or cancer diagnosis. We have successfully re-engaged well over 60% of these complex and sometimes hard to reach patients.”
This initiative, “Sustained 97% Opt-Out HIV Testing in the Emergency Department: Getting to Zero AIDS,” could well help the UK eliminate HIV infections entire by 2030, Cormack believes.
Enhancing Personalized Care for Heart Failure Patients
Heart failure is a chronic disease and a leading cause of hospitalization and 30-day readmissions in the United States. Acute and post-acute patient management pathways have been well documented for improved and enhanced patient care.
To improve care of heart-failure patients, a multidisciplinary clinical care team at Prisma Health, Greenville Memorial Hospital, created an initiative focused on identifying heart failure patients earlier, improving access to and utilization of limited resources, and reducing the overall cost of care.
This was accomplished through a patient identification and workflow program that used inherent capabilities of the electronic medical record (EMR) and integrated IT systems to identify and improve access for patients with increasing risk and advanced risk for heart failure.
Under this new program, heart failure patients are risk-stratified with deployment of real-time, point-of-care decision support and workflow, enabling improvement to care coordination and helping ensure the right provider sees at-risk hear failure patients at the right time.
The risk-score model uses laboratory results and is updated on an ongoing basis so that risk profiles used by clinicians are current.
Implementation of this EMR registry risk score resulted in a reduction in overall mortality, reduced length of stay, increased rates of high severity patients seen by the advanced heart failure specialty clinic, improved collaboration of clinicians for management of heart failure inpatients, and improved patient and family referrals, said Sandi Stoudenmire, director of cardiovascular services at Prisma Health.
“Broad adoption of this methodology demonstrated significant impact in the care of heart failure patients at our facility and can become a powerful tool for other disease states in the future,” she said.
The use of risk scoring in the electronic medical record yielded a 48% increase in the number of high-risk patients actively receiving care from an advanced heart failure specialist. Access to these specialists is limited by the number of available appointments, and the population of heart failure admissions in the facility increased 18% between 2020 and 2021. By matching resources to risk score, the most vulnerable patients have access to the specialty, Stoudenmire noted.
Prisma Health also saw a 12% improvement in overall mortality for all registry patients with heart failure. The post-registry mortality rate for high-risk registry patients is now approximately half that of patients with heart failure who during the same timeframe (September 2020 through August 2021) were not triaged and treated in accordance with the registry. In addition, use of risk scoring led to a 200% increase in referrals for palliative care and a 40% increase in hospice care referrals.
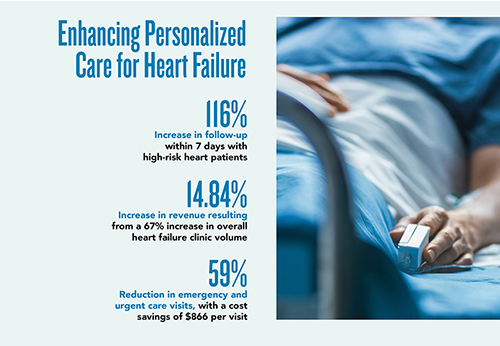
Since implementation of the heart failure registry, there is increased frequency of follow-up in patients of high severity, specifically a 116% increase in patient follow-up within 7 days. This improved post-discharge care of heart failure patients helps reduce readmissions, according to Stoudenmire.
Improved use of the EMR risk score to drive appropriate referrals at discharge also resulted in a 67% increase in overall heart failure clinic volume, which also increased revenues by almost 15%. In addition, a 59% reduction in average emergency and urgent care visits resulted in cost savings of about $866 per visit.
The initiative, which Stoudenmire describes as highly unique, was only moderately difficult to implement. “The development of the heart failure registry and addition of the patient risk-score within the provider’s daily work involved a small group with a passion to improve care through the enhancement of patient identification and personalization,” she said. “This work included automated referrals to the advanced heart failure team at the appropriate phase of a patient’s care, both acute and post-acute, in addition to referrals to the palliative care team and hospice and referrals for low- to medium-risk patients to the transitions clinic at discharge.”
The initiative, “Enhancing Personalized Care for Heart Failure Patients: A Risk-Scoring EMR Model,” is also highly scalable, Stoudenmire said, noting that it is serving as a model for other complex disease states in the development of the EMR.
Making a Difference in Patients’ Lives
Detecting disease and chronic conditions early enough to have a significant effect on patient outcomes is essential to improving the health of populations. These interdisciplinary initiatives, though relatively simply in nature, have had a demonstrable impact on patient care and outcomes, from prompt treatment for HIV to earlier discharge from the hospital to personalized care for patients at risk for heart failure.
These are just a few of the projects in which integrated care teams including the clinical laboratories are transforming healthcare delivery. To learn about other initiatives recognized through the UNIVANTS of Healthcare Excellence program, go to www.univantshce.com.
Kimberly Scott is a freelance writer who lives in Lewes, Delaware. +EMAIL: [email protected]
Univants 2021 Teams Recognized In This Issue
Utilizing an Innovative Approach to Process Improvement in the Era of a Global Pandemic and The Great Resignation: Rapidly Improving Timeliness of Laboratory Test Results for Multidisciplinary Rounds in an Acute Care Setting
Banner Health and Laboratory Sciences of Arizona, Sun City West, Arizona, United States
Kimm Wuestenberg
Connie Morena
Timothy Hersom
Kevin Cruz
Teri Dahn
Enhancing personalized care for Heart Failure Patients: a Risk-Scoring EMR model
Prisma Health Greenville Memorial Hospital, Greenville, South Carolina, United States
Beth Wehlitz
Jason Guichard
Stephanie Flippin
Beverly Jameson
Sandi Stoudenmire
Sustained 97% Opt-Out HIV Testing in the Emergency Department: Getting to zero AIDS
Croydon University Hospital, Croydon, Surrey, United Kingdom
Andrew Widdowson
Mike Bell
Leslie Parry
Ian Cormack
Sarah Horne
Linda Cheyenne Vaccari
See the full supplement.