For 2 years, everyone on planet earth has watched what is arguably the biggest global emergency in over a century unfold before our eyes. SARS-CoV-2, COVID-19, mRNA, “flattening the curve,” and other medical and laboratory jargon has become mainstream vocabulary. The pandemic of our generation has ebbed and flowed as most microbial outbreaks do, while humankind has experienced anxiety, heartbreak, hope, and exhaustion. Then, just as the world was beginning to hope for a pandemic ending, an old zoonotic agent reared its viral head: monkeypox.
The Current Outbreak
A confirmed case of monkeypox in the United Kingdom was reported on May 7, 2022. Cases have since popped up globally, from Spain and Germany to the U.S. and Canada. As of June 17, the U.S. reported 113 laboratory-confirmed cases in 20 states and the District of Columbia. Data from the World Health Organization (WHO), Centers for Disease Control and Prevention (CDC), and other public health authorities now indicate more than 1,300 confirmed monkeypox cases in 31 countries.
WHO is working with these countries, and others, to expand surveillance and provide guidance for monitoring and managing this outbreak. CDC scientists and others are tracking cases that have been reported in several countries that don’t normally report monkeypox, including the U.S. Historically, this infection is acquired via close contact (skin to skin or skin to fomites, such as bed linen), animal exposure, or more rarely via respiratory droplets. Interestingly, early data with this outbreak suggest that gay, bisexual, and other men who have sex with men make up most cases. However, most experts believe this is due to close contact and not a classically defined sexually transmitted infection.
What Is Monkeypox?
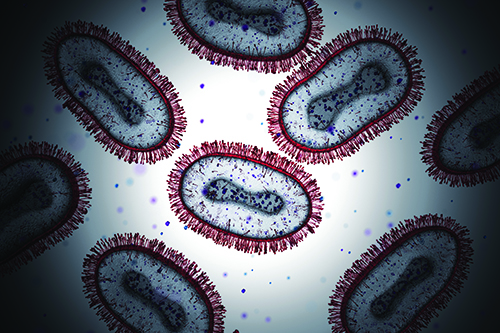
What exactly is monkeypox, and should we be concerned about the latest pathogen to capture headlines? The monkeypox virus is taxonomically in the Orthopoxvirus genus in the Poxviridae family, including smallpox and cowpox. Like all poxviruses, monkeypox virions are large, enveloped, and “brick-shaped.” Encapsulated within each virion is a core containing a linear, double-stranded DNA genome and enzymes required for virus uncoating and replication.
Monkeypox is a misnomer because monkeys are not the main reservoir. A more well-suited name would be “rodent pox” since the virus is believed to mainly reside in rodents (e.g., squirrels and rats). While several rodent species are suspected to be susceptible to monkeypox, the virus has only been isolated from wild animals on two occasions: a rope squirrel (1985) in the Democratic Republic of Congo and a dead infant mangabey monkey in Cote d’Ivoire (2012).
Transmission of monkeypox virus to and between humans occurs when individuals contact an infected animal, person, or contaminated material (fomites). In addition to gaining entry to the body via broken skin (including wounds invisible to the naked eye), the virus can travel in large respiratory droplets via the mouth, nose, or eyes. Because droplets are weighty, and fail to fly more than a few feet, prolonged contact is required for efficient human-to-human spread. In other words, monkeypox is nothing like SARS-CoV-2, which is aerosolized and highly transmissible.
Monkeypox is a self-limiting disease resolving within 2−4 weeks. Incubation is between 5 and 21 days so variation often occurs in individuals experiencing symptoms. In early stages, monkeypox illness may present like influenza, resulting in fever, headache, muscle aches, and swollen lymph nodes, among other symptoms.
First, a rash forms, blooming on the face before spreading to other body regions, including the palms (hands) and soles (feet). Rash lesions progress in stages, starting as macules (flat lesions), progressing to pustules (raised lesions filled with yellowish fluid), and ending in scabs, which eventually fall off. These symptoms mirror those of smallpox, though less severe, and most people recover without issue. Additionally, unlike monkeypox, smallpox is not associated with lymphadenopathy.
Monkeypox has a fatality rate ranging from 1%−10%. Case severity in individuals depends on several factors, including viral strain, medical care access and quality, exposure extent, and health status, such as being immunocompromised.
Currently there are two known virus clades: the more virulent Congo Basin clade (up to 10% mortality) and the less virulent West African clade (up to 1% mortality). So far, all confirmed monkeypox cases belong to the West African clade. To date, all nonendemic countries, including the U.S., report no mortality. Due to its low mortality rate, low reproductive number (Ro less than 1), transmission route (nonaerosol), and longer exposure time required for infection, monkeypox is very unlikely to become a pandemic or major problem. Food and Drug Administration-approved antivirals and vaccines are available.
Laboratory Detection of Monkeypox
Monkeypox is a very rare infection, especially in the U.S., and diagnosis is challenging, given that signs and symptoms mimic many other diseases. To diagnose suspected cases of monkeypox, clinicians rely on real-time quantitative PCR (RT-PCR) assays using sample material from skin lesions. Testing is performed at Laboratory Response Network (LRN) laboratories in the U.S. and globally. No commercial assays exist to detect monkeypox virus. There are approximately 120 domestic LRN laboratory members, representing all 50 states. Additionally, the LRN includes several international laboratories. Most current LRN members are public health laboratories.
If possible, successfully vaccinated (i.e., smallpox vaccination within the past 10 years) persons should perform laboratory work that involves handling specimens that may contain monkeypox virus, but it’s not an absolute requirement. BSL-2 facilities with standard BSL-2 work practices should be used for typical laboratory and clinical work involving suspicious or confirmed cases.
CDC published on June 6 an RT-PCR procedure for laboratories interested in creating laboratory developed tests for the virus. The procedure includes sequence information for primer and probe development and cycling conditions, and is available at www.cdc.gov/poxvirus/monkeypox/lab-personnel.
Rodney E. Rohde, PhD, MS, SM(ASCP)CM, SVCM, MBCM, FACSc, is a Regents’ Professor, University Distinguished Professor, Honorary Professor of International Studies, Global Fellow, and chair in the CLS program, College of Health Professions; associate director of the Translational Health Research Center, Texas State University; and associate adjunct professor of biology, Austin Community College. +Email: [email protected]