 Image credit:
Sebastian Kaulitzki/Thinkstockphotos.com
Image credit:
Sebastian Kaulitzki/Thinkstockphotos.com
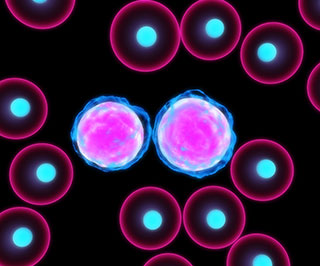
A study in the in the Journal of the American Medical Association (JAMA) suggests that mutations found through genetic profiling of bone marrow samples may provide the key to predicting relapse in patients with acute myeloid leukemia (AML).
Clinical outcomes for AML patients have improved due to the administration of certain treatments such as intensive chemotherapy and allogeneic stem cell transplantation. However, there’s been a lack of overall consistency in the prognosis for this disease, with at least 50% of patients relapsing and dying after receiving initial treatment. Just 20% recover completely, a related editorial in JAMA that discussed the findings noted.
A definitive test that predicts relapse in AML patients is currently out of reach, according to Timothy J. Ley, MD, a professor of oncology at Washington University School of Medicine in St. Louis, and the study’s senior author. “Such information is important to know because high-risk patients need aggressive, potentially curative therapy with a stem-cell transplant when they are in remission, early in the course of the disease,” Ley said in a statement from the university.
To determine the effectiveness of genetic profiling in assessing prognosis of AML patients, researchers employed whole-genome or whole-exome sequencing to do a retrospective analysis of bone marrow samples from 71 AML patients at different stages of the disease.
Sample analysis taken at diagnosis offered no new insights on a correlation between patient relapse after initial chemo treatment and the presence of leukemia-specific mutations. A more telling finding emerged when researchers analyzed the samples of 50 patients at the time of diagnosis and a month after chemotherapy, when these same patients were in remission.
Twenty-four patients representing 48% of all of the test subjects were found to have persistent leukemia-specific mutations in about 5% of their bone marrow cells, even though they were technically in remission.
Those whose mutations had persisted after chemotherapy had significantly lower median survival rates (10.5 months) versus the 26 patients whose chemotherapy treatment successfully cleared any mutations (42 months). This suggests that “the persistence of leukemia-associated variants approximately 30 days after initiation of chemotherapy was associated with an increased risk of relapse,” according to the study’s authors.
Those 26 in the cleared mutations group also had higher event-free survival rates (17.9 months) compared with the 24 patients in the persistent mutations group (6 months).
The study results “provide critical insights into the role of molecular monitoring in AML and into the dynamics of genetic mutations during AML treatment,” the JAMA editorial stated. It is the first study “to successfully use deep sequencing for the detection of persistent mutations in remission in AML, providing a path toward the use of next generation sequencing to follow patients with AML after initial therapy.”