Very small helms guide very large ships. Similarly, in vitro diagnostics account for only about 2.3% of healthcare expenditures in the U.S. but have an outsized influence on clinical decision-making (1). The enormous impact of diagnostics on patient health underscores the critical need to drive quality improvements with those who helm clinical genetic and genomic testing.
Unfortunately, test reimbursement is not well-aligned to promote accurate and useful genetic/genomic tests. Many health insurance companies, health systems, and employer benefit managers are unaware of the National Institutes of Health’s warning that “most genetic tests today are not regulated, meaning that they go to market without any independent analysis to verify the claims of the seller…[T]here is no federal oversight of the clinical validity of most genetic tests” (1).
In the U.S., clinical genetic and genomic testing labs provide diagnostic, predictive, prognostic, and theragnostic tests with perceived clinical value—a perception is frequently untethered from reality. This means that many patients are inadvertently harmed when well-meaning clinicians use low-value and inaccurate tests in patient care.
Some genetic tests cannot detect the mutations clinicians assume they can, as was recently reported for a Cowden syndrome family (2). Others might too readily and with insufficient evidence classify genetic variants as clinically meaningful, a problem featured in a 2019 Wall Street Journal report about a child’s ongoing diagnostic odyssey (3).
While most genetic/genomic test errors and deviations currently go undiscovered, published head-to-head comparison studies between labs often show low concordance, suggesting that fundamental technical issues plague the industry. Researchers at Vanderbilt undertook one such study, showing in 2016 only a 10% concordance in variant detection/classification on 63 persons with interesting genetic variants in only two cardiac genes when samples were tested at three different accredited laboratories (4).
What Is Value?
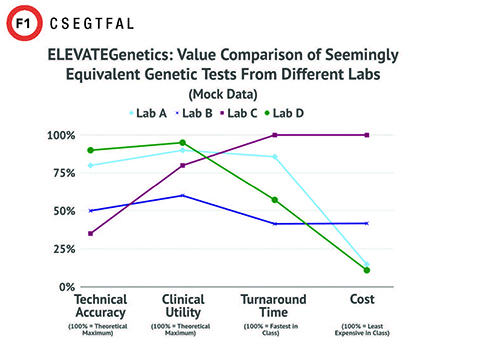
With mounting examples of genetic/genomic test discordance and failures, key stakeholders have begun looking for solutions to evaluate test value. The formula for measuring value of in vitro diagnostics uses measurements of clinical utility, cost, turnaround time, and technical accuracy (5). Turnaround time and costs can be determined readily, while a growing array of vendors provide as a service different measurements of clinical utility. However, comparative and standardized metrics of technical accuracy have been lacking. While CLIA certification or accreditation from an organization such as the College of American Pathologists is necessary to maintain minimal standards for laboratories, the scope of these accreditations does not consider all the critical aspects of technical accuracy that are important for accurate diagnosis and patient care.
Technical Accuracy
In clinical genetics and genomics, five major categories affect technical accuracy. Each poses for test results its own strengths, errors, and obstacles. The five categories include:
- personnel and laboratory accreditations;
- test ordering, sample tracking, and quality control;
- analytical validation and bioinformatics;
- variant classification; and
- test report content and organization.
Errors in any of these can have potentially devastating impacts on patients, including unnecessary surgeries, incorrect medications, misguided family planning decisions, or missed opportunities for early medical intervention. Table 1 offers several examples.
Quality Audits That Include Technical Accuracy
In conjunction with laboratory accreditation or test approval by the New York State Department of Health or the Food and Drug Administration, quality auditing can fill critical knowledge gaps for decisionmakers. The rapid evolution of the genetic/genomic diagnostic landscape outpaces accreditations and guidelines, which do not adequately address technical accuracy.
Therefore, the nonprofit and independent Center for Genomic Interpretation has developed a program that provides auditing services to stakeholders that includes technical accuracy, clinical utility, turnaround time, and cost measurements. This program, called ELEVATEGenetics (Figure 1), addresses the need for standardized and quantified metrics so that stakeholders—including consumers and insurers—have clear metrics by which to understand and compare the value of genetic and genomic tests.
Conclusion
As the clinical genetics and genomics industry continues to focus on making more clinically useful tests and aggressively solves technical accuracy problems, diagnostic value and downstream patient care will improve. We recommend that test accuracy and utility metrics be standardized and transparent, and that test reimbursement be tied to these metrics so that tests of higher value enjoy improved reimbursement rates.
Julie M. Eggington, PhD, is the co-founder and CEO of the Center for Genomic Interpretation in Sandy, Utah. Email: [email protected]
Megan E. Garlapow, PhD, is the chief strategy officer of the Center for Genomic Interpretation in Sandy, Utah. Email: [email protected]
References
- National Institutes of Health. National Human Genome Research Institute. Regulation of genetic tests. https://www.genome.gov/about-genomics/policy-issues/Regulation-of-Genetic-Tests (Accessed August 10, 2020).
- Ray T. Precision Oncology News. Genetic testing challenges in oncology: Assuming all labs are equal gives false reassurance of risk. https://www.precisiononcologynews.com/cancer/genetic-testing-challenges-oncology-assuming-all-labs-are-equal-gives-false-reassurance-risk#.XzGBxBNKh0t (Accessed August 10, 2020).
- Dockser Marcus A. The Wall Street Journal. The unfulfilled promise of DNA testing: Rapid advances in genetic testing are whipsawing families' diagnoses and treatment. https://www.wsj.com/articles/dna-testing-was-meant-to-help-treat-esmes-illness-it-created-turmoil-11558093193 (Accessed August 10, 2020).
- Van Driest SL, Wells QS, Stallings S, et al. JAMA 2016; 315:47-57.
- Rohr UP, Binder C, Dieterle T, et al. PLoS One 2016; doi:10.1371/journal.pone.0149856. Published correction PLoS One 2016;11:e0154008]
- Miller CE, Krautscheid P, Baldwin EE, et al. Am J Med Genet A 2014; 164A:1094-101.
- Lincoln SE, Zook JM, Chowdhury S, et al. Preprint in bioRxiv 2017; doi:10.1101/218529.
- Shah N, Hou YC, Yu HC, et al. Am J Hum Genet 2018;102:609-19.
- Mersch J, Brown N, Pirzadeh-Miller S, et al. JAMA 2018; 320:1266-74.