Big data and bioengineering advances are fueling rapid changes in diabetes technologies, which offer the promise of better self-management and quality of life for individuals with the disease, and easier care oversight by physicians. With the incidence of diabetes rising, these innovations are coming into use when “the ability of an individual living with diabetes to have human-to-human contact with their healthcare provider is not keeping pace with the number of people developing diabetes,” according to a recent review.
Continuous glucose monitors (CGM) and related sensor, pump, and information technologies have taken off, with patients embracing the empowerment they offer to self-track and manage glucose levels throughout the day. Between 30% and 40% of individuals with type 1 diabetes—and a growing number of those with type 2 diabetes—use CGMs. Manufacturers continue to refine these complex systems, but challenges remain around wider adoption and correct use of this evolving technology.
“These are mainly outpatient tools, and we’re not sure how useful they will be for treating patients,” said David Klonoff, MD, medical director of the Dorothy L. and James E. Frank Diabetes Research Institute of Mills-Peninsula Medical Center in San Mateo, California, and the founder and president of the Diabetes Technology Society. “The technology may turn out to be extremely useful. It’s under investigation right now.”
Demand Drivers
Several factors are pushing demand for CGMs and their associated systems, said Roman Hovorka, PhD, professor of metabolic technology at the University of Cambridge in the U.K. Patients and providers are looking for management devices that seamlessly pair glucose sensing and insulin delivery to control glucose levels more efficiently around the clock. These tools help individuals make better food and activity choices to better maintain normal glucose levels, he suggested.
Noninvasive convenience is also driving CGM use, according to Klonoff. Many patients struggle with gathering blood samples via fingerprick several times daily. This benefit also applies to other wearable technologies, such as patches and microneedle devices. “People don’t want to prick their fingers very much, and no one can prick their finger enough times a day to identify every time their blood sugar is too high or too low,” he said.
Improved connectivity and user experience also are prompting more people to jump aboard the CGM bandwagon. Bluetooth technology transmits glucose readings to patients’ smartphones which then transmit the data to electronic medical records for clinician review or to pediatric patients’ parents.
Current and Future Technologies
CGM products have been available for approximately 20 years, offering an alternative to standard blood glucose monitoring systems that rely on fingerprick samples. In recent years, they’ve improved in accuracy and ease-of-use, said Klonoff, though still need refinements.
Overall, CGM devices are considered either “open loop” or “closed loop” (Table 1). Open-loop monitors measure glucose levels subcutaneously at regular intervals, generally every 1 to 5 minutes. Users in most cases still have to self-check and calibrate their values via capillary blood glucose readings and adjust their insulin pump settings based on data from the monitor.

* Hybrid closed-loop system; functions as both insulin pump and continuous glucose monitor (CGM)
** Functions as both an insulin pump and a CGM, once integrated with the Dexcom G6 sensor and transmitter
a with Guardian Sensor 3
b with Enlite Sensor
c in individuals with type 1 diabetes
Sources:
American Diabetes Association Consumer Guide 2019 Continuous Glucose Monitors. http://main.diabetes.org/dforg/pdfs/2019/2019-cg-continuous-glucose-monitors.pdf
(Accessed September 2019).
diaTribe. Continuous Glucose Monitors https://diatribe.org/continuous-glucose-monitors (Accessed September 2019).
Diagnostics 2019;9: doi:10.3390/diagnostics9010031.
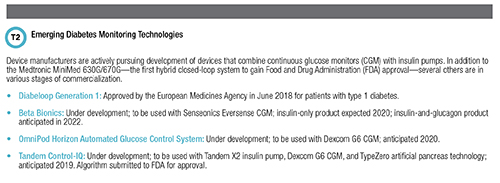
As well-accepted as open-loop systems are becoming, the future of CGM technology lies with closed-loop systems, also called an artificial pancreas, according to experts. Designed to mimic a healthy pancreas, these systems, only one of which—the Medtronic 670G—has been approved for use in the U.S., meld glucose sensing technology with insulin pumps (Table 2). Supported by special algorithms, they analyze glucose levels and determine appropriate insulin doses, which users need to check and confirm before they are administered. Single-hormone systems provide only insulin; double-hormone systems will offer insulin and glucagon.
For users, an artificial pancreas provides the full circle-of-care from immediate glucose management to clinician involvement, said Hovorka. “It’s the combination of more diabetes monitoring technologies and more collection of data that can be pushed into a system that can share information with healthcare professionals and with guardians and loved ones that is making these systems and devices as usable as possible,” he elaborated.
To that point, a recent American Diabetes Association review of diabetes technologies stressed that optimal use of either standard blood glucose monitoring systems or CGMs depends on both users and providers reviewing and interpreting these devices’ data output (Ann Intern Med 2019; doi:10.7326/M19-1638).
Ongoing work will make these systems smaller, Klonoff added, and they likely will deliver a more concentrated form of insulin currently under development. Additionally, future generation artificial pancreas systems will require fewer component replacements, fewer recalibrations, and less meal-time bolus insulin, predicted Natalie Allen, MD, a pediatric endocrinology and metabolism fellow at Virginia Commonwealth University in Richmond.
Challenges Ahead
According to Michael Hill, vice president of science, technology, and clinical affairs at Medtronic, the CGM market is currently growing between 20% to 30% annually, but the technology still presents challenges. “From customers, we always get feedback to make these tools smaller and last longer,” he said. “And there’s always the request to make them easier to use, particularly for kids and elderly patients.”
Like most new technologies, the devices can be cost prohibitive for patients who are un- or under-insured. Not only must they pay the initial sensor and transmitter costs, but they also shoulder the weekly, monthly, and yearly replacement expenses. These costs—and the projected benefits of CGM—would need to be weighed against the purchase of test strips for and level of glycemic control possible with standard blood glucose monitoring.
Additionally, interstitial glucose level measurements lag bloodstream measurements by approximately 10 minutes, and exercise can make it harder to secure accurate real-time readings, Allen cautioned.
A review Hovorka co-authored found that the latest sensor technologies have a mean absolute relative difference (MARD) versus lab-based tests of 8% to 14%, but that “accuracy is lower when measuring in the [hypoglycemic] range and when glucose levels are changing rapidly.” He added that with a MARD <10%, these systems are accurate enough “to allow patient self-adjustment of insulin dosage without confirmatory capillary blood glucose measurements” (Nat Rev Endo 2018;14:464-75).
Early studies of the Medtronic 670G hybrid closed-loop system show that users had improved HbA1c levels and time in range. However, research also suggests this technology is not a panacea: A small study of mostly pediatric patients found that nearly 40% stopped using this system mainly due to forced exits from the closed-loop automated basal delivery mode, frequent alarms, sensor supply and accuracy issues, and skin adhesion issues.
Cybersecurity involving CGMs is another concern, Klonoff said, because sensitive patient information is transmitted wirelessly to both families and clinicians. Further research is needed to ensure sufficient precautions exist to prevent data hacking.
In Hovorka’s view, perhaps the most dangerous challenge involves patients’ and families’ growing frustration with the progress of artificial pancreas development. Many have created do-it-yourself systems. In some cases, these closed-loop systems, pieced together with approved and unapproved components, have delivered unsafe amounts of insulin, and a case report of one system doing so prompted the Food and Drug Administration earlier this year to warn against their use. Consequent-ly, clinician-patient conversations about safety are critical, he emphasized.
Monitoring and Improving Performance
While CGM devices make it easier for patients to control their day-to-day glucose levels, this infor-mation is best viewed as a trend over time, said James Nichols, PhD, DABCC, FADLM, medical director of clinical chemistry and point-of-care testing at Vanderbilt University School of Medicine in Nashville. Because the values are based on interstitial fluid readings, they are less precise than clinical laboratory measurements and are not robust enough to be used in treatment decisions.
“It’s important from a laboratory perspective that we engage physicians and let them know that continuous glucose monitors are not laboratory devices,” he stressed, adding that clinical and laboratory staff should assume glucose monitoring for patients admitted to hospitals. “These devices are not quality controlled the same way a glucose meter or a core laboratory analyzer are.”
Consequently, he said, it’s incumbent upon clinical laboratory professionals to ensure physicians understand the margin-of-error and accuracy differences between CGM and lab-based methods. With that knowledge, clinicians can appropriately educate patients on the importance of being engaged in their own diabetes care, teaching them how to use CGM devices to monitor themselves and dose their own insulin.
Accuracy challenges, in fact, cover the gamut of diabetes self-monitoring technologies. Klonoff and Nichols co-authored a study that found that just six of 18 standard blood glucose meters cleared for personal use met a predefined accuracy standard on three of three studies, while four did not meet this standard on any of the studies (Diabetes Care 2018;41:1681-8).
Clinical laboratory professionals also should play a broader role in improving CGM performance by being part of CGM product development, suggested Ping Wang, PhD, DABCC, FADLM, associate professor of pathology and laboratory medicine at The Hospital of the University of Pennsylvania in Philadelphia. “CGM vendors should reach out to clinical laboratory professionals to build CGM devices with better accuracy,” she said. “Rather than conducting retroactive studies to determine ac-curacy, the industry should be more proactive. Collaborating with clinical professionals can improve accuracy during the early phases of product development itself.”
Even with some imperfections CGM devices are valuable tools for better managing glucose levels, she suggested. “In many cases, these devices can predict an upcoming drop in glucose, triggering an alarm for the patient,” she said. “Even though the tools aren’t as accurate, that’s a benefit that a clinical lab can’t offer.”
Conflicts of Interest:
Dr. Hovorka reports receiving speaker honoraria from Eli Lilly and Novo Nordisk and license fees from B Braun and Medtronic. He also serves on advisory panels at Eli Lilly and Novo Nordisk and is a consultant to B Braun.
Dr. Klonoff reports being a consultant for Abbott, Ascensia, Astra Zeneca, EOFlow, LifeCare, Merck, Novo Nordisk, Roche, and Voluntis.
Whitney J. Palmer is a freelance journalist in Holly Springs, North Carolina. +Email: [email protected]