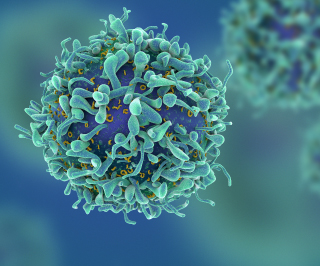
Image: Cgtoolbox / iStock
Clinicians for many years have relied on T cells engineered with disabled viruses to fight various kinds of cancer. Creating a viral vector is time consuming and challenging, however, and doesn’t always produce an ideal result. A team of scientists may have found an alternative: mixing a cocktail of T cells and DNA, applying some CRISPR–Cas9 gene editing magic and exposing all of the elements to an electrical field. The method makes it possible to insert large DNA sequences into specific areas of human T cells, affording those cells with new abilities to fight off disease.
An article in Nature describes how this new T cell approach was used in two separate experiments to kill melanoma cells and repair an autoimmune defect in children. “This is a rapid, flexible method that can be used to alter, enhance, and reprogram T cells so we can give them the specificity we want to destroy cancer, recognize infections, or tamp down the excessive immune response seen in autoimmune disease,” said the study’s senior author Alex Marson, MD, PhD, associate professor of microbiology and immunology at the University of California-San Francisco (UCSF), in a statement. “Now we’re off to the races on all these fronts.”
Marson and his colleagues anticipate that eliminating use of viral vectors could reduce genome targeting costs and improve safety, as well as speed up clinical applications and research. It took about a year for investigators to find the appropriate ratio of DNA and CRISPR allotments and T cell populations, applying all of these elements to electroporation, a process that temporarily relaxes cell membranes by exposing them to an electrical field. This enables T cells to integrate specific genetic sequences at the site where CRISPR–Cas9 made its “cut” in the genome.
After validating the nonviral genome-targeting system’s ability to label different types of T cell proteins, the investigators tested this approach in two scenarios. In the first experiment, they used it to repair a IL2RA mutation in cells from three siblings. The defect had afflicted the children with an autoimmune disease that hadn’t responded to therapy. The CRISPR technique not only corrected the defect but also restored faulty cellular signals caused by this mutation.
They also used this approach to replace the native T cell receptor (TCR) locus with a new one that redirected T cells to hunt down a specific subtype of melanoma cell. “The resulting TCR-engineered T cells specifically recognized tumor antigens and mounted productive antitumor cell responses in vitro and in vivo,” the authors summarized. Investigators tested this method in mice seeded with human melanoma tumors, observing that the engineered T cells were able to zero in on tumor sites and attack the cancer.
“This strategy of replacing the T cell receptor can be generalized to any T cell receptor,” said Marson, a member of the Parker Institute for Cancer Immunotherapy at UCSF. “With this new technique, we can cut and paste into a specified place, rewriting a specific page in the genome sequence.”
The approach also eliminates the need for a half-dozen people working with viruses in a lab to engineer T cells, according to the study’s first author Theo Roth, a student pursuing MD and PhD degrees in UCSF’s Medical Scientist Training Program. “If we begin to see hundreds of labs engineering these cells, working with increasingly more complex DNA sequences, we’ll be trying so many more possibilities that it will significantly speed up the development of future generations of cell therapy,” Roth said.
Looking forward, the research team plans to work collaboratively with different groups to develop new therapeutic strategies for cancer, autoimmune diseases, and infectious diseases. “There is much work ahead to determine the most effective genome modifications, develop clinical grade products, and test safety and efficacy,” Marson told CLN Stat.