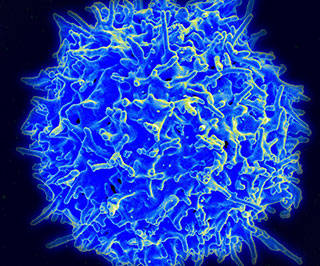
 Image credit: NIAID
Image credit: NIAID
A new immunotherapy method that infuses a patient’s own regulatory T cells, or “Tregs,” into his or her blood shows promise as a safe, effective treatment for type 1 diabetes (TD1), according to a study published in Science Translational Medicine.
As the researchers explain in their article, Tregs “have been shown to be defective in the autoimmune disease setting. Thus, efforts to repair or replace Tregs in T1D may reverse autoimmunity and protect the remaining insulin-producing β cells.”
Type 1 diabetics have typically received immunosuppressive drugs as therapy, yet the results from a trial that tested this “adoptive transfer” approach takes things in a new direction, said the study’s lead author, Jeffrey A. Bluestone, PhD, a metabolism and endocrinology professor at University of California, San Francisco, in a statement. “By using Tregs to ‘re-educate’ the immune system, we may be able to really change the course of this disease,” Bluestone said.
To test the adoptive transfer method, Bluestone and his colleagues in a phase 1 trial enlisted 14 adults between the ages of 18 and 43 with recent-onset T1D. Using an “isolation and expansion” method they had previously developed, the researchers took blood samples from the test subjects, segregated the Tregs from other cells in the blood, and then “grew” them in their lab.
The same study participants then received infusions of the heightened number of Tregs, some receiving higher doses than others. One group, for example, received 5 million cells, compared to another group that received up to 2.6 billion cells.
No matter the dose, all of the test subjects successfully tolerated the Tregs infusions. “Immune studies showed transient increases in Tregs in recipients,” according to the findings. They also discovered that these cells had staying power: 25% of the infused Tregs were still detectable a year later in some of the test subjects.
The expectation is this method could work in conjunction with other immunotherapy methods to treat TD1.
“Using a patient’s own cells–identifying them, isolating them, expanding them, and infusing them back into the patient–is an exciting new pillar for drug development…and we expect Tregs to be an important part of diabetes therapy in the future,” Bluestone said. Ultimately, the goal is to improve immunotherapy to the point that patients wouldn’t need to take insulin injections.