 Image credit: selvanegra/Thinkstock
Image credit: selvanegra/Thinkstock
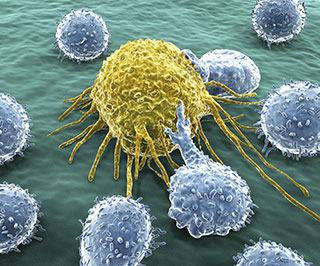
Immunotherapeutics are growing in importance as a weapon against cancer. A recent uptick in accelerated federal approvals for certain lung and deadly skin cancers underscores their role as anticancer agents.
On Oct. 2, the U.S. Food and Drug Administration approved the use of Keytruda (pembrolizumab) for treating advanced (metastatic) non-small cell lung cancer (NSCLC). This is specifically for patients whose cancer failed to respond to previous therapies.
Pembrolizumab in this instance acts as a companion diagnostic, meaning that patients must test positive for the protein PD-L1 to receive this treatment. “This is the first immunotherapeutic to be approved in conjunction with a companion diagnostic test, the PD-L1 IHC 22C3 pharmDx test, which can detect the presence of the protein PD-L1 in non-small cell lung tumors,” observes the American Association for Cancer Research (AACR), which has been chronicling the recent surge in immunotherapies as anticancer agents in a series of blog posts.
FDA approved pembrolizumab for advanced NSCLC following a randomized clinical trial of 550 patients with this disease. The study’s researchers determined that among a subgroup of 61 patients who were treated with pembrolizumab after previous therapies failed, more than 40% saw a reduction in their tumors, with treatment effects lasting 2 to 9 months.
With FDA’s approval of pembrolizumab, there are two classes of immune checkpoint inhibitors available for patients with NSCLC. Earlier this year nivolumab was approved for treating squamous NSCLC.
Pembrolizumab had previously been approved to treat metastatic melanoma following a patient’s treatment with the immunotherapy drug ipilimumab.
Ipilimumab in the meantime may now be used in combination with nivolumab to treat patients with BRAF V600 wild-type, unresectable or metastatic melanoma. FDA on Sept. 30 announced accelerated approval for this drug treatment combination. Individually, each of these drugs had already been approved to treat melanoma.
“Ipilimumab and nivolumab work in different ways to unleash a patient’s immune system. They release different brakes on immune cells called T cells, which have natural cancer-fighting potential. Given that the two immunotherapeutics release different brakes, CTLA-4 and PD-1, respectively, researchers tested the idea that combining them might be more effective than using them alone,” AACR wrote in a recent blog post.
A randomized clinical trial found that among 109 patients with BRAF V600 wild-type melanoma, the combination treatment ipilimumab/nivolumab reduced tumors in 60% of the test subjects, compared with just 11% who received ipilimumab on its own.
Severe adverse reactions, however, were more frequently reported in patients receiving the combination treatment.
F. Stephen Hodi, MD, director of the Melanoma Center at Dana-Farber Cancer Institute and associate professor of medicine at Harvard Medical School in Boston, brought up these concerns at the AACR annual meeting in April.
As reported in AACR’s blog, Hodi urged that the adverse effects associated with the ipilimumab/nivolumab treatment warranted further study.
“A phase III clinical trial, CheckMate67, which is comparing the ipilimumab-nivolumab combination with both ipilimumab and nivolumab monotherapy, is already well underway and should provide the answer as to whether the combination provides additional clinical benefit compared with the individual immunotherapeutics,” AACR’s blog post noted.