
For police, recognizing people affected by drug or alcohol consumption is complex and requires an ambitious classification process beyond noticing, for example, the odor of alcohol. Police worldwide have distinct methods to identify people under the influence in either traffic stops or after committing a crime.
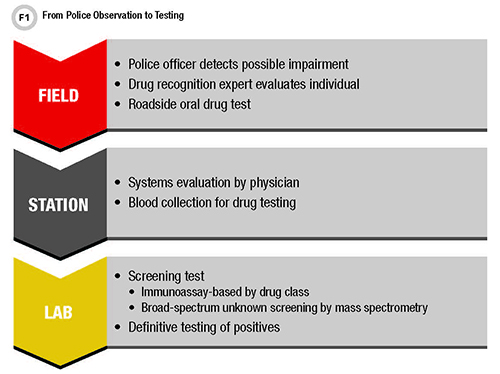
Beyond asking a person to perform psychophysical tests at a traffic stop, police use drug tests that offer clues about consumption. Depending on the country, police might emphasize one type of test or test medium over another. In Germany, the State Institute for Preventive Action and the Institute of Legal Medicine at Saarland University work on drug use detection strategies independent of drug tests. As a result, our researchers developed the method of unaffected observation (Figure 1) based on an escalating series of communication and recognition processes that police can use to classify a person as affected by a drug.
Active cooperation with traffic control personnel is voluntary in Germany, and our method is independent of the kind of substance involved. Since this method is based first on behavioral evaluation, no equipment is needed initially, but police need training before they use the method.
Changing the Old Strategy of Drug Recognition
A challenge for police is recognizing the effects of drugs so they know when to request testing. While a drug test helps detect affected persons, for police the process starts with the case background. For example, in individuals suspected of driving under the influence, detecting acute drug actions is important; thus, blood would be the specimen of choice. Police, however, cannot draw blood. This makes saliva a better sample type for on-site testing: Concentrations of drugs in saliva typically correlate well with blood, and the sampling technique is not invasive. Conversely, abstinence programs need to cover longer time periods. This makes urine the better matrix due to the prolonged detectability of drugs and their metabolites.
The convenience and rapid results of on-site testing make police more efficient. But there are disadvantages, too. These include personnel training and hygiene-related aspects of collecting a sample, the possibility that the person suspected of being under the influence might manipulate the specimen, and the potential for false-negative or false-positive results.
False-negative results typically happen when substances or classes of drugs are not covered by on-site tests (for example, new psychoactive substances or pharmaceuticals). Meanwhile, cross reactions of different substances with the screening tests lead to false-positive results.
Psychophysical testing presents another option in recognizing drug actions during traffic stops and other police interventions. These tests, originally used in Germany, enable police to evaluate shared attention through coordination of motion sequences, and tests of short-term memory, reaction capacity, and fine motor skills.
Examples include asking the individual to walk and turn around, stand on one leg, or perform with closed eyes finger-to-finger and finger-to-nose tests. Shared attention tests evaluate a person’s ability to capture and process different stimuli at one time and react appropriately. However, police need to be trained thoroughly before using them, as typically these tests would have been conducted by physicians.
A New Approach: Unaffected Observation
The method of unaffected observation exploits knowledge about drug actions. The central nervous system (CNS) is a highly complex structure that coordinates the perception, processing, and reaction of body functions. One part of the CNS—the sympathetic nervous system—is independent of a person’s will. Consequently, symptoms mediated through this system offer more objective evidence. Activation of the sympathetic nerve system—such as in a dangerous situation that mobilizes the flight response—can result in dilated pupils, dry mouth, restlessness, higher risk readiness, and other observable symptoms.
That said, an otherwise harmless interaction with police can be a reason for excitement. Police must separate natural anxiety from the effects of stimulant drugs like amphetamine, cocaine, or others. Police officers can recognize these basic flight symptoms without performing drug tests or psychophysical tests, which again, are voluntary in Germany after the person has been cautioned. The goal of unaffected observation is to conduct a 3-minute conversation that calms natural stress and allows the police officer to recognize drug symptoms objectively.
When a police officer initiates unaffected observation, the goal is to recognize and assemble mosaic parts of the sympathetic CNS response without the subject’s active cooperation (Figure 1). When this observation yields enough evidence of impairment, there is no need to perform a drug test. However, when partial evidence of drug effect exists, but the police officer is unsure, he or she can offer a drug test to substantiate drug use and order a blood draw.
The following three case reports show how neither unaffected observation nor drug tests alone can prevent the need for a blood draw, but act as different pieces of the mosaic of drug recognition.
Case 1: A Disoriented Woman
A 49-year-old female was stopped by a drug recognition expert (DRE) in a police check. She seemed to be uncoordinated, confused, and disoriented. Her reactions were delayed and her speech was slurred. She staggered and her pupils were constricted. Because the woman appeared to be under the influence of drugs, the DRE offered a saliva drug test for cannabinoids, amphetamines, designer amphetamines, opiates, cocaine, benzodiazepines, and methadone; this test was negative for the included substances.
The DRE then called a physician to draw a blood sample. The physician arrived at the police station 2 hours later and recognized considerable influence of alcohol, drugs, or other medications. Signs included high-frequency nystagmus, disconnected thought, excessive talkativeness, and depressive mood. The blood sample was analyzed for psychoactive substances, starting with immunoassay-based prescreening for classic drugs (i.e., benzodiazepines, opiates, amphetamines, designer amphetamines, cannabinoids, cocaine, methadone, and buprenorphine). All of these were negative, so the specimen was then assessed with a general unknown screening assay using gas chromatography-mass spectrometry (GC-MS). Liquid-liquid extraction in native as well as acetylated extracts was required to screen for at least 10,000 different substances. Diphenhydramine, zopiclone, and trace ibuprofen were ultimately identified in the serum sample, which was then subjected to quantitative measurement in a separate liquid chromatography MS (LC-MS/MS) test. Quantitative testing revealed concentrations of 0.4 mg/L diphenhydramine and 0.7 mg/L zopiclone. Compared with reference data, these concentrations fall at therapeutic and supra-therapeutic levels, respectively (1).
Diphenhydramine is an antihistamine used for short-term treatment of sleeping disorders. Side effects can be somnolence, drowsiness, concentration disorder extending to the following day after intake, visual disturbances, and paradoxical reactions including arousal and anxiety. Zopiclone is a short-acting sedative, typically used as a hypnotic agent. Expected side effects are similar to benzodiazepines (i.e., delayed reaction, somnolence, dizziness, confusion, affected muscle function, diminished ability to concentrate, visual disturbances, and/or amnesia). In combination with other CNS depressant substances, enhanced interactions are possible. Given these findings, the symptoms could be explained due to the action of the proven medications, which means that the driver committed a traffic offense.
Case 2: A Man With Aggressive Behavior
A 19-year-old male stopped by the police had the following symptoms: heavy swaying and disturbed equilibrium, extremely delayed reactions, restlessness, babbling speech, drowsiness, confusion, depressed mood, obtrusive and aggressive behavior, dizziness when leaving the car, and requiring support when walking. His pupils were unresponsive to light, and the young man was somnolent and apathetic during the drive to the police station. A saliva drug test was positive for benzodiazepines. A physician came to the police station 2 hours later and recognized a considerable influence of alcohol, drugs, and/or medications with low-frequency nystagmus, unsafe straight walking with staggering, unsafe U-turn with staggering, unsafe standing on one leg, stupor, and disturbed orientation. A blood sample was collected and analyzed in a similar way as described in Case 1, using immunoassay for classic drugs, general unknown screening with GC-MS, and multi-target screening with LC-MS/MS. This testing detected tramadol and flualprazolam; quantitative assessment with LC-MS/MS revealed a concentration of 0.065 mg/L flualprazolam and trace tramadol (i.e., below the limit of quantitation).
Flualprazolam is a derivative of alprazolam, a benzodiazepine used to treat states of arousal, anxiety, and stress. However, flualprazolam is a new psychoactive substance, sold as a legal high via the Internet and not requiring a prescription. Similar to alprazolam, flualprazolam induces strong hypnotic, anxiolytic, and sedative actions. Studies have shown that fluorinated analogs of benzodiazepines are often more potent than unfluorinated analogs (2). Compared with the therapeutic concentration of alprazolam (1), the measured flualprazolam concentration in this case fell in an upper therapeutic level. Thus, the symptoms could be explained due to the action of the proven benzodiazepine detected in the blood sample, which means that the driver committed a traffic offense.
Case 3: A Man With Slurred Speech
An 18-year-old male was stopped with noticeable problems at a police check and was detained. His thinking routine was delayed, and his speech was slurred. He did not understand questions unless asked repetitively. He was restless, and his legs and fingers showed tremor. His mood was notably depressed, and his gait was unsafe and wobbly. Also, his eyelids fluttered, and he swayed while standing with closed eyes. His face was pale, he had dry mouth, and his pupils showed a delayed reaction to light.
A saliva drug test performed in the presence of the police revealed negative results for classic drugs. An hour later, a physician determined as minor the influence of alcohol, drugs, or medication. Nevertheless, he observed unsteady walking, unsafe finger-finger and finger-nose tests, delayed thinking, as well as depressed mood. A blood sample analyzed as described in cases 1 and 2 identified the synthetic cannabinoid JWH-210, and quantitative LC-MS/MS testing revealed a concentration of about 0.17 ng/mL.
As a synthetic cannabinoid, JWH-210 theoretically has the same effects as cannabis—particularly, tetrahydrocannabinol (THC) and other bioactive intermediates. These effects include disturbances in judgment and the ability to take criticism, altered mood and actuation, and thought disorder. Lack of interest and general slowdown are further effects to be expected from cannabinoids, as well as diminished attention and concentration. Also, perception and spatial orientation can be affected. Overdose can lead to tachycardia, hallucinations, and panic attacks. Due to the stronger binding of JWH-210 to the cannabinoid receptor compared with THC, JWH-210 has a higher potential for toxic effects. In this case, the symptoms were consistent with a lower-level exposure to JWH-210, which means that the young man committed an offense.
Conclusion
The foundation for the police to order blood samples from drivers in Saarland, Germany, rests on them recognizing sympathetic CNS symptoms that might be explained by the action of psychoactive substances. On-site drug testing is just one piece of the puzzle to prove a drug action, but it is limited to certain drug classes. Thus, even negative pretests cannot prevent a blood draw when a police officer recognizes symptoms of drug action in a detained individual. Labs should use comprehensive screening and quantitative confirmation methods to cover as many psychoactive substances as possible and should enable a forensic toxicologist to examine each case.
Hans-Juergen Maurer is a police officer retiree at the State Institute for Preventive Action in Saarland, Germany.
Harald Frey is a police officer at the State Institute for Preventive Action in Saarland, Germany.
Nadine Schaefer, PhD, is deputy head of forensic toxicology at the Institute of Legal Medicine at Saarland University in Germany.
Andreas H. Ewald, PhD, is a forensic toxicologist (GTFCh) and head of forensic toxicology at the Institute of Legal Medicine at Saarland University in Germany. +Email: [email protected]
References
- Schulz M, Iwersen-Bergmann S, Andresen H, et al. Therapeutic and toxic blood concentrations of nearly 1000 drugs and other xenobiotics. Crit Care 2012;26:16:R136.
- Hester JB Jr, Rudzik AD, Kamdar BV. 6-phenyl-4H-s-triazol[4,3-a][1,4]benzodiazepines which have central nervous system depressant activity. J Med Chem 1971;14:1078-8