Do you have any advice on how to think systematically about maintaining quality laboratory operations when an institution’s IT systems are down? What are the main risks that laboratory managers need to mitigate? Anything that helps staff prioritize their work would be particularly helpful to me!
A Concerned Laboratory Manager
 Respondent
Respondent
Nikola Baumann, PhD
Director of the Central Clinical Laboratory
and Central Processing
Mayo Clinic
Rochester, Minn.
IT downtime is a universal challenge for clinical laboratories, medical centers, and healthcare systems. In the laboratory, we rely heavily on information systems and electronic interfacing between multiple systems to support the entire testing process from ordering to reporting. A recent article in the New England Journal of Medicine focused on the importance of this topic in the context of electronic health records (EHR) and the Joint Commission's National Patient Safety goals (1). The authors proposed a three-phase framework for developing EHR-specific patient safety goals. Phase 1 specifically addresses safety concerns and reducing the effects of IT downtime on clinical operations and patient safety.
The Expected and Unexpected
There are two types of situations laboratories should be prepared for: planned outages for hotfixes, updates, or upgrades; and unexpected failures or impairments of unknown duration. In either case, it is essential to have robust backup plans and comprehensive standard operating procedures for handling these in a manner that maintains critical operations at near optimal levels, does not compromise patient care, and ensures patient safety.
Workflow often changes dramatically when IT systems are down. All or any of the following may be impacted or impaired: physician ordering; sample collection and labeling; receiving and testing specimens in the laboratory; and reporting results. Laboratories that operate in paperless, automated, electronically-interfaced environments must resort to manual or paper reporting. Furthermore, staffing shortages may also contribute to challenges in the normal workflow.
Creating the Plan
The first step toward handling IT downtime successfully is having a clear activation and communication plan, as well as criteria for when downtime procedures should be initiated. Laboratory managers should consider outages to all types of systems, including computerized physician order entry (CPOE), laboratory information systems, middleware, and EHRs, as well as the entire network. Downtime procedures may vary slightly depending on which systems are impacted during the outage; however, it is important to keep the process as consistent and simple as possible so that staff can remain competent and responsive without having to account for too many deviations.
Downtime plans should also be shared with patient care areas to ensure that they account for the total testing process. In some situations, clinical services may initiate downtime procedures when either CPOE or EHR access is impaired. Communication trees work well and allow patient care areas to have a single laboratory contact as well as to ensure smooth inter- and intra-laboratory communication. Likewise, it is valuable to have a mechanism in place for proactive communication to all providers when laboratory systems are unexpectedly down. A brief mass communication stating that laboratory results will be delayed can prevent numerous unnecessary phone calls to the laboratory.
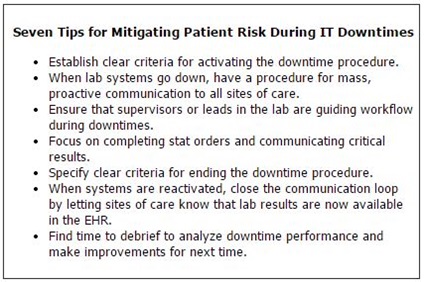
Forming a command center during unplanned IT outages may help facilitate prompt, situation-specific decision-making. Furthermore, laboratory managers may find it useful to have a designated lead technologist or supervisor who can help prioritize work and direct traffic. Clear criteria for when to initiate procedures, such as when a system has been down for 30 minutes, will help laboratory staff stay on top of incoming work. Without such criteria, laboratory staff may delay initiating downtime procedures during an unexpected outage, because both they and IT staff are optimistic that the system will be functional soon. Ten minute intervals can quickly turn into hours, and once a backlog of specimens accumulates, it is more difficult for the laboratory to recover. When there are clear procedures, communication, and directives, laboratory staff can focus on doing the work and worry less about putting out fires.
STAT testing orders from the emergency department (ED) or intensive or critical care units should be the highest priority during IT downtimes. Simple visual cues like colored labels or stickers can be very helpful for organizing and prioritizing sample flow. For example, if the labels on specimens coming from the ED are yellow or have a colored sticker, they can be easily routed to appropriate testing areas. Specimen collection areas must also ensure that downtime labeling, whether printed or handwritten, is consistent and contains two appropriate identifiers.
Critical result reporting should be a special focus of risk mitigation during IT outages. When everything is functioning normally, the LIS or middleware programs typically identify these results and trigger critical result reporting. For laboratories with call centers, remote locations and individuals outside the laboratory may even report critical results. During IT outages affecting these systems, laboratory staff must assume the responsibility of both identifying critical values and, as appropriate, verbally reporting them to providers. In addition, care providers must have mechanisms for receiving and documenting critical results when the EHR is down. Again, it is important to work as a team with patient care areas as they may opt to set up clinical service command centers or use designated service pagers for receiving critical result information during outages.
Back to Paper Reports
Frequently, laboratories choose to revert to paper-based systems during IT downtimes, in which case results are printed, faxed, or sent via courier or pneumatic tube to clinical units. Depending on how your laboratory generates reports, results originating from chemistry, hematology, or microbiology laboratories may be formatted differently.
It is helpful to standardize the laboratory result reporting as much as possible. A laboratory report template that includes patient identifiers, test names, and reference intervals with standard formatting makes it easier for care providers to quickly and accurately identify the patient and relevant laboratory test results during potentially stressful working conditions that are more vulnerable to errors. Labs might even consider limiting the test menu that is available during downtimes to support the most essential laboratory testing.
Returning to Normal
Even after systems become functional again, while orders and results are downloading or systems are recovering, there may be a lag time before the laboratory is operating normally. The information system may be live, but it is vital to communicate with end-users prior to returning to routine operation. For example, the final step of the laboratory's downtime procedure might be to call the ED, verify that results are available electronically, and confirm that delivery of paper reports will be discontinued. This simple step of closing the communication loop is especially important when reactivating after an IT outage. Similar communications between ordering, collection, and receiving areas should be built into the laboratory's procedure.
Regroup and Assess
Finally, it is useful to regroup after a major outage. Review what went well and what could be improved, and continue to refine the workflow and procedures. In our laboratory we learn something new from each downtime and make efforts toward better communication and more seamless processes.
REFERENCE
- Sittig DF, Singh H. Electronic health records and national patient-safety goals. N Engl J Med 2012;367:1854–60.