
During the past decade, understanding of and treatments for osteoporosis have advanced significantly, opening the door for greater use of bone turnover markers, and underscoring the need for more robust measurement of these analytes. Researchers now know much more about bone biology and have parlayed that, along with large-scale prospective population studies, into more precise measurements for bone mineral density, common diagnostic criteria, and better specification of clinical risk factors for osteoporosis. These milestones have been coupled with increased use of drug therapies to manage the disease. As the science in these areas has progressed, researchers and clinicians have come to recognize the emerging role of bone turnover markers, and with it, the benefits of standardizing measurement of these important analytes. Progress toward this goal will be discussed at today’s Morning Symposium, "Bone Marker Standards in Osteoporosis," taking place from 9:30 a.m.–12:00 p.m. in Room 408A of the Los Angeles Convention Center.
"What's happened is there's increasing awareness that bone turnover markers have a unique role to play in helping healthcare providers predict fracture risk independent of bone mineral density. They also show us the pharmacodynamic response of osteoporosis treatment, and are helpful in monitoring patients," explained Stuart Silverman, MD. "However, practitioners, including myself, have been somewhat hesitant in the past to use these markers because there's been inadequate measurement control, limited data comparing the impact of bone turnover changes with treatments over time, and a lot of variability, both biological and analytical."
Silverman, who is medical director for the Bone Center of Excellence at Cedars-Sinai Medical Center in Beverly Hills, Calif., will moderate today's session, which will feature an international panel of experts who will discuss recent developments in the use of bone turnover markers and progress towards standardizing their measurement. The session is being cosponsored by the International Federation of Clinical Chemistry and Laboratory Medicine (IFCC) and the International Osteoporosis Foundation (IOF), which have a very active Working Group on the Standardization of Bone Marker Assays (See Box, below).
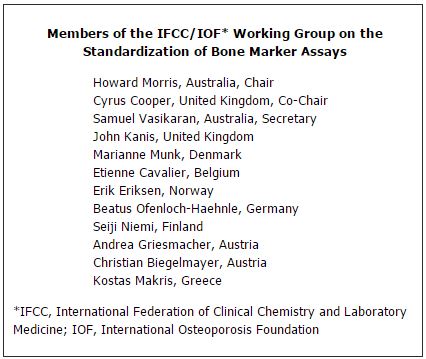
Joining Silverman will be the chair and two members of the IFCC/IOF Working Group. The chair of the group, Howard Morris, PhD, FAACB, ARCPA, will discuss plans and progress in standardizing bone marker assays. He is chief medical scientist in chemical pathology at SA Pathology and professor of medical sciences at the University of South Australia in Adelaide. Panelist Cyrus Cooper MA, DM, FRCP, will address the health impact of osteoporosis as well as methods for assessing fracture risk. Cooper holds joint appointments as professor of epidemiology at the University of Oxford and as professor of rheumatology and director of the MRC Epidemiology Resource Centre at the University of Southampton in the U.K. The role of bone turnover markers in osteoporosis will be the focus of Samuel Vasikaran, MBBS, MSc, MD, FRCPA, head of core clinical pathology and biochemistry at Royal Perth Hospital and clinical professor of medicine at the University of Western Australia in Perth.
Establishing Reference Markers
The IFCC/IOF Working Group already has taken important steps towards achieving standardization of bone turnover markers. Of particular note, the group in 2011 issued a position paper that reviewed the evidence for bone turnover markers in predicting fracture risk and in monitoring osteoporosis therapy, and presented priorities for future research (Osteoporos Int 2011;22:391–420). The group also recommended as reference markers serum procollagen type I N propeptide (S-PINP) and serum C-terminal telopeptide of type I collagen (s-CTX), as indicators of bone formation and bone resorption, respectively. "Whilst no perfect gold standard marker exists, these were chosen based on a number of criteria. These include adequate characterization and clear definition of the marker; their specificity for bone and performance in clinical studies; wide availability; biological and analytical variability; sample handling; stability; ease of analysis and availability of method in routine laboratories; and the medium of measurement—urine versus serum," said Cooper at the time the recommendations were published.
Looking forward, the IFCC/IOF Working Group has several projects underway to advance the standardization initiative. Among other activities, the group is reviewing the literature and current status of available assays to establish a reference measurement system for standardization or harmonization of s-CTX and S-PINP assays, as well as considering critical decision limits and potential target levels for these two analytes.
Silverman explained that research and clinical care have been hampered for want of robust analytics involving bone turnover markers. "Right now there are multiple markers, but we want to try to get the same markers used everywhere for all clinical trials. Bone turnover markers have not been included in fracture risk algorithms because of the scarcity of population-based studies with any single analyte. So establishing S-PINP as the marker for formation and s-CTX as the marker for absorption would be a good starting point," he said. "We'd like to identify biases for the assays, and try to have them all report the same reference ranges with similar units. Even the procedures need to be harmonized. Here in the U.S. for example, bone turnover markers are sometimes done on serum, sometimes on plasma, but we would want them always done on plasma tubes."
The Working Group's literature review found 17 different bone turnover markers used in clinical trials, with up to 10 evaluated in any given study. There was considerable heterogeneity in fracture outcomes reported, and inconsistency in the predictive value of specific markers, ranging from strong to non-significant. The authors also found variability in the analytic methods used, with outcomes varying depending on the method used. For example, undercarboxylated osteocalcin was significantly associated with fracture risk when measured by immunoassay, but not when there was a hydroxyapatite binding step. The Working Group also emphasized that time of day is critical to the level of some bone turnover markers (See Table, below).
|
Sources of Pre-Analytical Variability in Measuring Bone Turnover Markers
|
|
Uncontrollable Sources
|
Controllable Sources
|
Age
Menopausal Status
Sex
Fractures
Pregnancy and Lactation
Drug Therapy
Disease
Bed Rest/Immobility
Geography
Ethnicity
Use of Oral Contraceptives |
Circadian Cycles
Fasting Status
Exercise
Menstrual Status
Seasonal
Diet |
| Source: Adapted from Osteoporos Int 2011;22:391–420 |
Questioning the Role of Bisphosphonates
The Working Group's efforts took on added urgency in May when the New England Journal of Medicine published a Food and Drug Administration analysis of the efficacy of bisphosphonates, the popular bone-building medications approved for treatment of osteoporosis (N Engl J Med 2012;366:2048–2051). The review, launched in response to postmarketing reports of rare but serious adverse events associated with the drugs, found little if any benefit from the medications after 3-5 years. The authors fell short of making specific recommendations, but many in the osteoporosis community believe the findings could sharply curtail use of the drugs, and place a premium on bone turnover marker testing.
"In reaction to this study, a lot of patients are being put on holiday from these drugs, but physicians need markers to know when they should put patients back on these medications or on new medications. So there's a real clinical need to have markers right now," explained Silverman. He also pointed out that many payers, Medicare included, cover only biennial bone density scanning, posing a dilemma for women and their physicians in terms of decision-making around the use of bisphosphonates. "Let's say we discover you have osteoporosis. Would you personally take a medication for two years knowing the first time I as your physician could give you any information about the effectiveness of that medicine is two years from now?" he said. "This is an expensive medication, and you're reading in the news media that it has side-effects and people are stopping taking it. This is where we need these bone turnover markers, because I can measure them within three months after you start the medication and see whether or not the medication is working."
Attendees at today's Symposium will hear a full airing of the challenges and controversies in the field. Silverman also hopes they will be inspired to become involved in bone turnover marker standardization efforts.