A 51 year old patient with increasing generalised weakness and shortness of breath for the last four months was admitted to hospital for further evaluation. On admission his serum creatinine was 3.1 mg/dL(elevated), the BUN was 46 mg/dL (elevated) and the complete hemogram showed a haemoglobin of 7.9 gm/dL (low) with the peripheral blood smear revealing a normocytic normochromic type of anemia. He was diabetic and was well controlled using oral medications. His blood pressure was normal. His urine protein was 2+ by dipstick. His serum electrolytes were within normal limits. Due to the presence of impaired renal function, serum calcium and phosphate were ordered. The calcium was 10.1 mg/dL (RI: 8.5-10.5 mg/dL) and serum phosphate was 24.8 mg/dL (RI: 2.5-4.5 mg/dL). Serum phosphate was rechecked and the results were similar. Is such elevation in serum phosphate possible and what could be the reason for such an extreme degree of hyperphosphatemia ?
In the absence of phosphate poisoning, such an elevated serum phosphate level is essentially impossible physiologically. Spurious elevations in phosphate can be termed "pseudohyperphosphatemia."
Paraproteinemia is a common cause of analytical interferences leading to spuriously elevated phosphate. Considering this possibility, we measured the total serum protein and albumin and calculated the albumin-to-globulin ratio. The total protein was 11.4 gm/dL (greatly elevated) and the albumin was 2.3 gm/dL (low).This prompted us to perform a serum electrophoresis which revealed an band of restricted mobility in the gamma globulin fraction (refer to figure). The patient sample was then assayed for phosphate by serial dilutions. There was complete lack of linearity in the phosphate results suggesting an analytical interference. This issue was discussed with the treating physician and the diagnosis of multiple myeloma was confirmed by bone marrow examination. An X-ray of the skull revealed a punched out lytic lesion typical of multiple myeloma. Immunofixation was done which show an IgG kappa monoclonal M-spike. The serum IgG was 11,580 mg/dL (RI: 450-1500) while the other immunoglobulins were within the reference intervals.
IgG kappa is well known to interfere with the phosphomolybdate principle used in the assay of serum phosphate on most automated chemistry analysers [1]. Our phosphate result was obtained on a Olympus analyser but similar results were found on a Roche platform. All “wet” chemistry analysers will probably exhibit this interference in the phosphate assay. We then send out this sample for phosphate measurement using a dry chemistry analyser (Vitros) and the result was within the reference interval. The BaSO4 spreading layer present in the Vitros dry chemistry slide filters the protein in serum and assays phosphate in a protein free filtrate. This prevents the positive interference of the IgG kappa monoclonal gammopathy. For labs which do not have a dry chemistry system, a serial dilution analysis of the suspected analyte could be performed. Lack of linearity is an indirect indicator of potential interference.
Interferences are always problematic in clinical chemistry. Proper recognition of such interferences can lead to the diagnosis of disorders like paraproteinemia as was found in this case. Proper communication between laboratorians and clinicians is necessary to solve such interesting clinico – biochemical issues.
References:
- Hawkins RC. Pseudohyperphosphataemia in multiple myeloma. Ann Clin Biochem. 1991 May;28 ( Pt 3):226-8.
General references:
Sonnenblick M, Eylath U, Brisk R, Eldad C, Hershko C. Paraprotein interference with colorimetry of phosphate in serum of some patients with multiple myeloma. Clin Chem 1986;32:1537-1539.
Yang Y, Howanitz PJ, Howanitz JH, Gorfajn H, Wong K. Paraproteins are a common cause of interferences with automated chemistry methods. Arch Pathol Lab Med 2008;132:217–23.
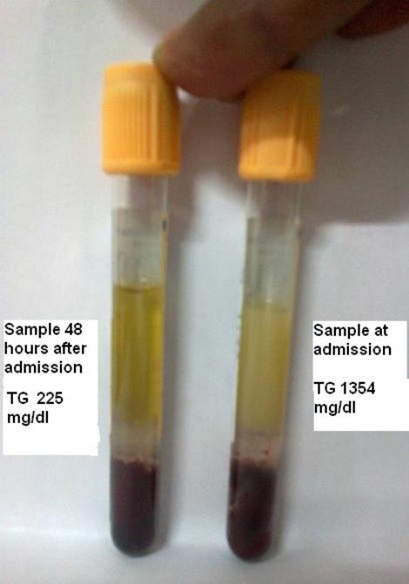
Figure: