Case: The patient was an African American woman between the ages of 30 and 40 years. She previously had a gastric bypass and lost weight from 400 lbs to less than 200 lbs. Since that time the patient suffered from multiple episodes of ill defined abdominal pain, vomiting and diarrhea attributed, in part, to abdominal abscesses that were treated with antibiotics.
Presently the patient was admitted from the emergency room with the chief complaint of "generalized body pain" of one day's duration although abdominal pain was her greatest complaint. She provided a past history of sickle cell disease. Her medications included oxycodone, Percocet (acetaminophen and oxycodone), carisoprodol (a muscle relaxant), alprazolam (a benzodiazepine) and zolpidem (a sedative that is used for the short-term treatment of insomnia).
Her CBC displayed a normocytic anemia [RBC count : 3.6 mill/uL (reference interval: 4.0 - 5.2 mill/uL); Hemoglobin: 10.5 g/dL (reference interval: 12.0 - 16.0 g/dL); Hematocrit: 33% (reference interval: 35 - 45%) and MCV: 91.2 fL (reference interval: 78.0 - 100.0 fL)]. The WBC count was low at 2,300/uL (reference interval: 4,000 - 10,000/uL). As well, the platelet count was low at 133,000/uL (reference interval: 150,000 - 450,000/uL).
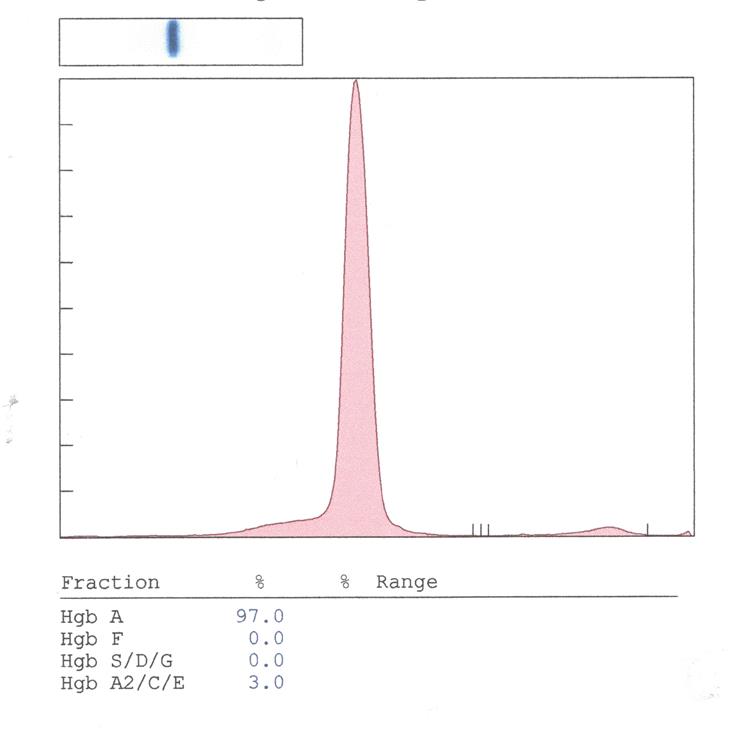
Hemoglobin electrophoresis was ordered to confirm the patient's past history of sickle cell disease. The hemoglobin electrophoresis gave the following results (note: the migration locations of abnormal hemoglobins and A2 are depicted for reference):
How would you proceed?
The work-up for the patient's abdominal pain was negative. AST, ALT, lipase and amylase were normal and a CT scan of the abdomen was normal. Her stool studies for infectious agents were negative.
Her symptoms resolved with conservative management (npo, IV fluids and then po fluids and food). The patient asked for IV pain medication initially but that was slowly weaned back to oral pain medications. On the third hospital day she was discharged.
Draw while the patient was hospitalized, the hemoglobin electrophoresis was normal. A sickle cell solubility test done the following day was negative. With 2 tests consistent with no hemoglobin S done on different days in the in-patient setting, it is highly unlikely that these were mis-labeled samples.
The discordance between the patient's history of sickle cell disease and the laboratory results suggests several possibilities. For example, the patient may not have been correctly advised as to the cause of her anemia by her health care providers (although this is unlikely). Alternatively, she may have misunderstood what was told to her.
Of concern is that the patient exhibited "pain medication seeking behavior" (taken verbatim from the discharge note). This assessment was based upon the patient constantly requesting pain medication. Furthermore, it was determined that the patient had multiple pain medication prescriptions being filled with overlapping dates. From this one can theorize that the patient feigned sickle cell crises to obtain prescriptions for opiates.
Of interest, this patient’s medications list included carisoprodol, an opioid (oxycodone) and a benzodiazepine (alprazolam). The use of these 3 drugs together is sometimes referred to as the “holy trinity” in drug abuse parlance (1,2). Apparently this combination can produce an euphoric sensation similar to that of heroin.