[Download PDF]
Executive Summary
The clinical laboratory continues to play a critical role in managing the coronavirus disease 2019 (COVID-19) pandemic. Currently, molecular testing is the method of choice for detection of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) in respiratory specimens and diagnosis of active infection. Over the past several months, numerous serologic tests have become available. Notably, both the performance characteristics of these assays and their clinical utility continue to be defined and are evolving in real-time during this pandemic. Interim guidelines for appropriate serologic test utilization and interpretation have been published by multiple professional organizations. However, no guidelines to date provide comprehensive, literature-based recommendations for laboratory professionals who are directly involved in the selection, validation, implementation, and quality management of Food and Drug Administration (FDA) emergency use authorization (EUA) or laboratory developed tests (LDTs) in clinical laboratories. Building on the the Association for Diagnostics & Laboratory Medicine (formerly AACC) position statement entitled “the Association for Diagnostics & Laboratory Medicine (ADLM) Recommendations for SARS-CoV-2 Serology Testing”, we convened a panel of experts from clinical chemistry, microbiology, and immunology laboratories. This group also includes experts from the in vitro diagnostics (IVD) industry and regulatory agencies. The outcome is these expert-based practical recommendations to support laboratory professionals in implementing serologic testing amidst the rapidly-evolving COVID-19 pandemic.
The currently available serologic tests and platforms with FDA EUA are presented, including a discussion of neutralizing antibody (nAb) assays. Additionally, information on serologic assay design, antibody classes (i.e., IgM, IgG, IgA, total immunoglobulins), and the kinetics of the humoral immune response are provided. Verification and validation of both EUA and LDTs are described, with a focus on the number and type of samples required, selection of patient populations, design of cross-reactivity studies and acceptability criteria, among other topics.
Four indications for serologic testing are discussed: 1) supporting the diagnosis of COVID-19 and related sequelae (i.e., multisystem inflammatory syndrome in children [MIS-C]), 2) identifying potential convalescent plasma donors and manufacturing of convalescent plasma, 3) epidemiologic and seroprevalence studies, and 4) vaccine efficacy studies. This document summarizes the utility of serologic testing for each of these indications and provides detailed information that may aid laboratorians when discussing serologic assay selection and implementation with clinical colleagues.
Recommendations for quality management, result interpretation, reporting comments, and the role of orthogonal testing are also outlined.
Introduction
As of November 7, 2020, over 50 million cases and 1 million deaths have been reported to the World Health Organization (WHO) worldwide as a result of COVID-19. In the United States, over 9.5 million confirmed cases and 234,000 deaths were reported to the WHO1. COVID-19 is caused by SARS-CoV-2, a member of the genus Betacoronavirus (Beta-CoV) and a close relative of severe acute respiratory syndrome (SARS) coronavirus (CoV) and Middle East Respiratory Syndrome MERS-CoV2,3. Other genus members include the seasonal human CoVs OC43 and HKU1.
While molecular testing, including real-time reverse transcription polymerase chain reaction (RT-PCR) performed on respiratory specimens is routinely used for diagnosis of active infection with SARS-CoV-2, serologic testing is used to determine recent or previous antibody immune response to the virus.
Rapid development and implementation of SARS-CoV-2 antibody assays has been ongoing during the pandemic. Typically, commercially-produced IVD assays undergo thorough evaluation by the FDA before distribution to clinical laboratories. However, during an emergent national or international outbreak, the Secretary of Health and Human Services (HHS) may declare a public health emergency, which under section 564 of the Federal Food, Drug and Cosmetic Act4 allows the FDA to grant EUA of unapproved medical products or devices for the purpose of diagnosing, treating, or preventing the disease (Table 1).
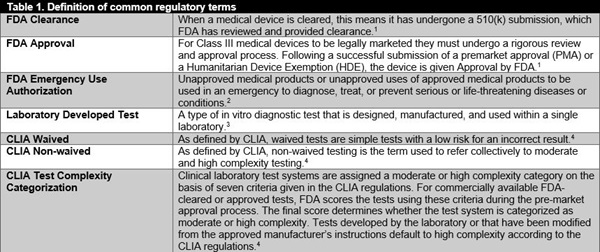
FDA, Food and Drug Administration; CLIA, Clinical Laboratory Improvement Amendments
Table legend: This table provides a list of common definitions regarding regulations in the United States.
Reference:
1https://www.greenlight.guru/blog/fda-clearance-approval-granted;
2https://www.fda.gov/emergency-preparedness-and-response/mcm-legal-regulatory-and-policy-framework/emergency-use-authorization;
3https://www.fda.gov/medical-devices/vitro-diagnostics/laboratory-developed-tests#:~:text=A%20laboratory%20developed%20test%20(LDT,used%20within%20a%20single%20laboratory;
4https://www.cdc.gov/clia/test-complexities.html#:~:text=As%20defined%20by%20CLIA%2C%20waived,the%20FDA%20for%20home%20use.
The HHS Secretary issued a public health emergency declaration for SARS-CoV-2 on January 31st, 2020. Notably, while the FDA immediately required EUA for SARS-CoV-2 molecular tests, EUA was only recommended for serologic assays because such tests were not considered diagnostic, and per the FDA, were intended to only be used for seroprevalence and epidemiologic studies. This lenient regulatory environment for serologic assays led to the development and availability of over 200 antibody tests for SARS-CoV-2, of which 53 have obtained EUA as of October 20, 2020. Unfortunately, multiple reports began emerging of serologic assays with poor performance characteristics or lack of appropriate validation, prompting the FDA to update their policy on May 4th, 2020 to require EUA for all commercially available serologic assays5. The FDA also provided a list of serologic assays that should not be distributed or used due to either poor performance or lack of EUA submission. Importantly, the FDA reserved the right to revoke EUA status at any time should evidence of poor assay performance be documented. To date, EUA status has been revoked for 2 previously authorized serologic tests6–8.
As a result of the limited FDA oversight of serologic tests, as well as due to incomplete understanding of kinetics, relevance, and durability of humoral immune response in COVID-19, questions have arisen in the clinical community on how to best utilize these assays as well as result interpretation in management of patients. In an effort to provide assistance for such scenarios, a panel of clinical diagnostic laboratory and industry experts from across North America reviewed the current literature to provide expert opinions on how to best implement these assays to support patient care needs.
This manuscript provides the most up-to-date understanding of host immune response to SARS-CoV-2, the associated antibody kinetics, and the currently available assays with EUA. Clinical utility and assay limitations are discussed to help laboratories select the appropriate test(s) for their purposes and targeted population needs. The process and considerations necessary to verify or validate either EUA or LDT serologic tests in a clinical setting are described. In addition, test interpretation, orthogonal testing strategies, and issues of laboratory biosafety are outlined. It is the intention of this document to provide a comprehensive reference for laboratory professionals and healthcare workers to appropriately implement these assays in the clinical laboratory and interpret the results to serve their patient needs during this pandemic. Additionally, given the more frequent occurrence of outbreaks associated with either vector-borne (e.g., Zika virus, dengue virus, etc.) or respiratory pathogens, this document will be a useful resource in planning for similar scenarios in the future.
[Read the Full PDF]