Summary
DOI: 10.1373/clinchem.2018/291344
A 17-year-old, 6-week pregnant female presented to the emergency department with symptoms of abdominal pain, nausea, and vomiting for 2 days.
Student Discussion
Student Discussion Document (pdf)
Grace R. Williams1,2 and Robert D. Nerenz1,2*
1Department of Pathology and Laboratory Medicine, Dartmouth-Hitchcock Medical Center, Lebanon, NH; 2The
Geisel School of Medicine at Dartmouth, Hanover, NH.
*Address correspondence to this author at: Department of Pathology and Laboratory Medicine, Dartmouth-Hitchcock
Medical Center, Lebanon, NH 03756. Fax 603-650-7214; e-mail [email protected]
Case Description
A 17-year-old, 6-week pregnant female presented to the emergency department with symptoms of
abdominal pain, nausea, and vomiting for 2 days. Although she initially complained of only low right
abdominal pain, by the next day, she complained of a generalized abdominal ache. Laboratory values
upon admission included a plasma sodium concentration of 118 mmol/L, potassium of 3.0 mmol/L,
and chloride of 80 mmol/L. On the third day of admission, she experienced 2 seizures. She denied
previous history of seizures or other neurological diseases, but she did have a long history of
“eczema-like” rashes on her face, neck, and hands that had been unresponsive to prednisone. A urine
drug screen was negative, and physical examination was unremarkable. On review of her chart, it
was noted that 6 months before her hospital admission, the patient had consulted a dermatologist
who described numerous small eroded papules and scarring on the back of the patient’s hands, neck,
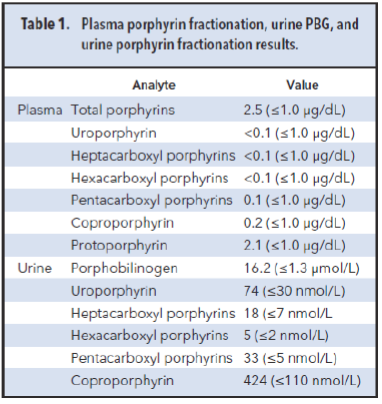
and upper chest. Urine and plasma specimens collected during this dermatology appointment had
been sent to a reference laboratory for porphyrin fractionation and porphobilinogen (PBG)
measurement. Results are presented in Table 1. Because of the patient’s symptoms upon
presentation to the emergency department and previously increased urine PBG concentration, she
was treated with daily hemin infusions for 4 days and her symptoms resolved. Over the consequent 2
days, her plasma sodium concentration increased to 135 mmol/L and she was discharged.
Questions to Consider
- What are some causes of concurrent hyponatremia and abdominal pain?
- How would acute porphyria be differentiated from other conditions with a similar clinical presentation?
- Why did the patient’s symptoms resolve following hemin infusion?
- How should molecular testing be integrated into the further workup of this patient?
Final Publication and Comments
The final published version with discussion and comments from the experts appears
in the June 2019 issue of Clinical Chemistry, approximately 3-4 weeks after the Student Discussion is posted.
Educational Centers
If you are associated with an educational center and would like to receive the cases and
questions 3-4 weeks in advance of publication, please email [email protected].
AACC is pleased to allow free reproduction and distribution of this Clinical Case
Study for personal or classroom discussion use. When photocopying, please make sure
the DOI and copyright notice appear on each copy.
DOI: 10.1373/clinchem.2018/291344
Copyright © 2019 American Association for Clinical Chemistry