Summary
DOI: 10.1373/clinchem.2019.301572
A 25-year-old woman presented to the emergency department with a 1-day history of nausea, fatigue, exertional lightheadedness, and a syncopal event without witnessed seizure activity or urinary incontinence.
Student Discussion
Student Discussion Document (pdf)
Monica R. Hill, Mark R. Hopkins, and Claire E. Knezevic*
Department of Pathology, The Johns Hopkins University School of Medicine, Baltimore, MD.
*Address correspondence to this author at: 1800 Orleans St, Zayed B1–1020G, Baltimore, MD 21287. Fax +410-955-0767; e-mail [email protected]
Case Description
A 25-year-old woman presented to the emergency department with a 1-day history of nausea, fatigue, exertional lightheadedness, and a syncopal event without witnessed seizure activity or urinary incontinence. The patient had a past medical history of fibromyalgia and nonepileptiform seizure disorder, and she was prescribed oxycodone for use as needed (although she reported as
“not really taking”) and ibuprofen for pain. She denied use of any other medications, illicit substances, or herbal supplements. Her family history was negative for cardiac problems or history of sudden death.
At presentation, her blood pressure was 75/42 mmHg; heart rate was 61 beats/min (intermittently
dropping to the 30s); temperature was 36.3 °C (97.3 °F), respiration was 16 breaths/min; and oxygen saturation was 99% by pulse oximetry. Her physical examination was remarkable for ongoing near-syncopal events and an irregular cardiac rhythm with variable S1 and S2 without
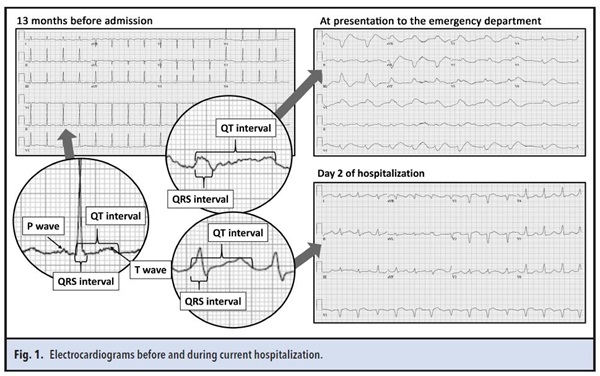
murmurs, rubs, or gallops. Initial electrocardiogram (ECG) showed bradycardia with a wide-complex rhythm and QTc prolongation to 554 ms (Fig. 1). Two prior ECGs within the past 2 years had shown normal sinus rhythm with normal intervals.
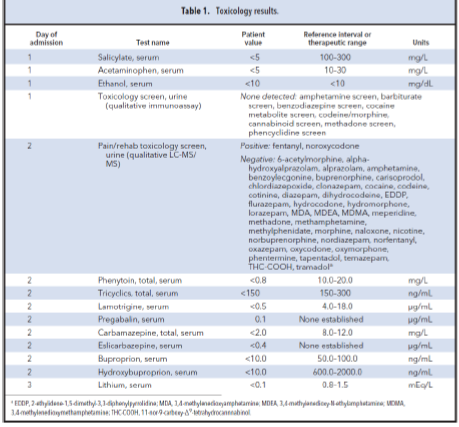
On admission, initial chemistries were within the reference range except for a serum creatinine concentration of 1.6 mg/dL (increased from a baseline of 0.9 mg/dL), and serum and urine toxicology tests were negative (Table 1). A complete blood count showed a normocytic anemia at the patient’s baseline: hemoglobin was 10.8 g/dL (reference interval, 12.0 –15.0 g/dL) and mean corpuscular volume was 89.5 fL (reference interval, 80.0–100.0 fL). Thyroid function testing, electroencephalogram, and head computed tomography were unrevealing. A transthoracic echocardiogram was remarkable for abnormal septal motion consistent with a conduction abnormality. Continuous intravenous isoproterenol was initiated to induce tachycardia and shorten the QTc interval, and intravenous sodium bicarbonate was empirically started to counteract possible ingestion of sodium channel– blocking agents. The patient continued to deny substance ingestion, and subsequent serum and urine testing on days 2 and 3 of hospitalization was negative with the exception of fentanyl, which she received in the emergency department, and noroxycodone, a metabolite of her prescribed oxycodone (Table 1). She became more alert in appearance, but ECGs continued to show a wide QRS (up to 192 ms) and prolonged QTc intervals (up to 739 ms) with alternating left bundle branch block and right bundle branch block morphologies despite
continuous isoproterenol and sodium bicarbonate infusions (Fig. 1).
Questions to Consider
- What is the differential diagnosis for a patient with a prolonged QT interval?
- What are the appropriate initial steps in evaluating patients with a suspected toxidrome?
- What is the clinical value of send-out toxicology testing?
Final Publication and Comments
The final published version with discussion and comments from the experts appears
in the November 2019 issue of Clinical Chemistry, approximately 3-4 weeks after the Student Discussion is posted.
Educational Centers
If you are associated with an educational center and would like to receive the cases and
questions 3-4 weeks in advance of publication, please email [email protected].
AACC is pleased to allow free reproduction and distribution of this Clinical Case
Study for personal or classroom discussion use. When photocopying, please make sure
the DOI and copyright notice appear on each copy.
DOI: 10.1373/Clinchem.2007.097139
Copyright © 2019 American Association for Clinical Chemistry