Summary
DOI: 10.1373/clinchem.2017.279430
Student Discussion
Student Discussion Document (pdf)
Naga Yalla*
Division of Endocrinology, Metabolism, and Lipid Research, Washington University, St. Louis, MO.
*Address correspondence to this author at: Washington University in St. Louis, Campus Box 8127, 660 South Euclid Ave., St. Louis, MO 63110-1093. Fax 314-262-7641; e-mail [email protected]
Case Description
A 58-year-old Caucasian woman was referred to the University Bone Health Program for evaluation. Her past medical history was significant for Roux-en-Y gastric bypass (RYGB) surgery 10 years previously, following which she lost 100 pounds, but she regained weight
thereafter, for a net weight loss of 20 pounds (current body mass index 44 kg/m2). In addition, she had a history of hypothyroidism, osteoarthritis, and esophageal ulcers. Eight months before her visit, she sustained bilateral pubic rami fractures following a fall from standing height. A few months later, she complained of worsening pelvic pain. At that time, a magnetic resonance image revealed sacral insufficiency fractures. She was diagnosed
with vitamin D deficiency (25-OH vitamin D concentration <13 ng/mL [30–100 ng/mL]) and hypocalcemia (total serum calcium 8.1 mg/dL [8.6 –10.4 mg/dL] with normal serum albumin). She had been taking 1200 mg of calcium citrate per day, but 50000 IUs of vitamin D (cholecalciferol) once weekly was prescribed in addition. On the basis of a presumed diagnosis of osteoporosis, she was also prescribed 150 mg of ibandronate (Boniva®)
once monthly.
Her reproductive history included menarche at age 14 and a hysterectomy at age 33, for which she had taken hormone replacement therapy ever since (Premarin® 1.25 mg daily). Other pertinent medications included omeprazole (a proton pump inhibitor).
A review of systems was positive for a constellation of symptoms, including diffuse dull aching bony pain, fatigue, decreased muscle strength, and increasing gait instability
with frequent falls.
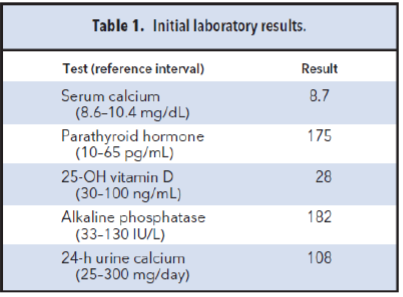
Her laboratory tests revealed a microcytic anemia, with subsequent iron studies confirming iron deficiency. Pertinent laboratory test results are listed in Table 1. Of note, her vitamin B12, vitamin A, folic acid, and zinc concentrations were within the respective reference intervals.
Bone densitometry determined by dual-energy x-ray absorptiometry revealed the following T-scores: lumbar spine (L1–L4) was -0.7, total hip was -1.2, and left femoral neck was -1.2. For diagnostic purposes, values above -1.0 are considered normal, from -1.0 to
-2.5 suggest osteopenia, and less than -2.5 suggest osteoporosis.
Obesity has emerged as a global epidemic. In the US alone, 1 in 20 adults suffers from extreme obesity, defined as a body mass index >40 kg/m2 (1) Bariatric surgery has emerged as an effective treatment for patients with severe obesity, often producing durable weight loss and attendant improvements in the metabolic complications associated with obesity (including hypertension, diabetes mellitus, and obstructive sleep apnea), as well as a
decrease in mortality.
Bariatric surgery procedures are generally classified as being restrictive (e.g., sleeve
gastrectomy and adjustable gastric banding) or malabsorptive [e.g., biliopancreatic
diversions (BPD)]. RYGB is considered to be a combination of restrictive and malabsorptive
procedures.
The RYGB involves the creation of a 30-mL proximal gastric pouch that is anastomosed
directly to the proximal jejunum, thus bypassing the greater portion of the stomach and
duodenum. This results both in a narrow anastomotic outlet, which serves to restrict caloric
intake, and a substantial decrease in the intestinal surface area available for caloric
absorption. In the long term, however, the procedure often results in the malabsorption
of necessary minerals and fat-soluble vitamins (2).
Sleeve gastrectomies are a relatively new procedure, but have surpassed RYGB as the
most popular bariatric technique (3). Though bariatric surgery appears to be beneficial
from a cardiometabolic standpoint, there is emerging concern regarding the negative
impact of these surgeries on long-term skeletal health, particularly malabsorptive and
mixed procedures like RYGB. Recent studies have demonstrated an increase in bone
turnover markers and declines in bone mineral density following these procedures (2, 4).
Initially, bone loss was attributed primarily to nutritional deficiencies (which can range
from malabsorption to frank osteomalacia) and the effects of skeletal unloading due to
weight loss. However, in the last decade, pioneering work by bone biologists has pointed
to a complex “cross talk” among adipocytes, the skeletal system, and the gastrointestinal
system. These neurohormonal changes have been implicated as potential mediators of
bone loss (2, 4).
References
- Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the
distribution of body mass index among US adults, 1999 –2010. JAMA 2012;307:
491–7.
- Folli F, Sabowitz BN, Schwesinger W, Fanti P, Guardado-Mendoza R, Muscogiuri G.
Bariatric surgery and bone disease: from clinical perspective to molecular insights. Int
J Obes 2012;36:1373–9.
- Estimate of Bariatric Surgery Numbers, 2011–2015. American Society for Metabolic
and Bariatric Surgery. https://asmbs.org/resources/estimate-of-bariatric-surgerynumbers
(Accessed March 2017).
- Yu EW, Bouxsein ML, Roy AE, Baldwin C, Cange A, Neer RM, et al. Bone loss after
bariatric surgery: discordant results between DXA and QCT bone density. J Bone Miner
Res 2014;29:542–50.
Questions to Consider
- What is the most likely diagnosis in this patient?
- What mechanisms explain the effects of bariatric surgery on skeletal health?
- What is the best long-term management of this patient?
Final Publication and Comments
The final published version with discussion and comments from the experts appears
in the January 2018 issue of Clinical Chemistry, approximately 3-4 weeks after the Student Discussion is posted.
Educational Centers
If you are associated with an educational center and would like to receive the cases and
questions 3-4 weeks in advance of publication, please email [email protected].
AACC is pleased to allow free reproduction and distribution of this Clinical Case
Study for personal or classroom discussion use. When photocopying, please make sure
the DOI and copyright notice appear on each copy.
DOI: 10.1373/clinchem.2017.279430
Copyright © 2018 American Association for Clinical Chemistry