Summary
DOI: 10.1373/clinchem.2017.274720
A 31-year-old Chinese woman with bilateral upper extremity swelling presented to the emergency department at the 20th week of gestation. According to the patient, “normal fetal movement” had stopped 3 days before admission.
Student Discussion
Student Discussion Document (pdf)
Yanhong Zhai,1† Wei Song,2† Jiazi Zeng,1 Zhen Zhao,3 and Zheng Cao1*
1Department of Laboratory Medicine, Beijing Obstetrics and Gynecology Hospital, Capital Medical University, Beijing, China; 2Department of Obstetrics and Gynecology, Beijing Obstetrics and Gynecology Hospital, Capital Medical University, Beijing China; 3Department of Laboratory Medicine, Clinical Center, National Institutes of Health, Bethesda, MD.
*Address correspondence to this author at: Department of Laboratory Medicine, Beijing Obstetrics and Gynecology Hospital, Capital Medical University, 251 Yaojiaoyuan Road, Beijing, China 100026. Fax +86 10-52276; e-mail [email protected].
† Y. Zhai and W. Song contributed equally to this work, and both should be considered as first authors.
Case Description
A 31-year-old Chinese woman with bilateral upper extremity swelling presented to the emergency department at the 20th week of gestation. According to the patient, “normal fetal movement” had stopped 3 days before admission. No abdominal pain or obvious vaginal bleeding was noted. Her body temperature was 36.5 °C and blood pressure was 110/70 mmHg with a heart rate of 80 beats/
min. However, there was no fetal heart rate or movement that could be detected by ultrasonography examination, suggesting spontaneous abortion. Although there was no significant family history, the patient had 1 stillbirth 3 years ago at 27 weeks of gestation, accompanied by eclampsia before her labor induction.
Because her fetus showed no signs of life with ultrasonography examination, the patient agreed to have ethacridine (Rivanol)-induced labor on day 3 of her hospitalization. On the day of her induction, her blood pressure went up to 158/82 mmHg with proteinuria (urine chemistry: protein +4) and low platelet count (90 X 109/L, normal range 100–300X109/L), consistent with a diagnosis of preeclampsia. Magnesium sulfate was administrated during and after the delivery for seizure prophylaxis. After delivery, her blood pressure decreased to 133/81 mmHg and other preeclampsia symptoms resolved in the next few days before discharge.
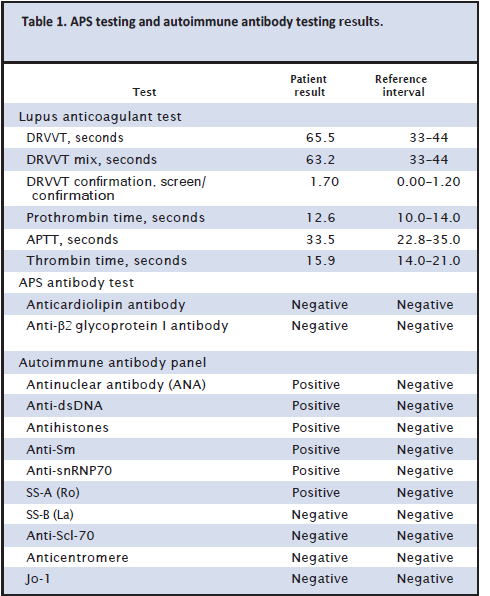
According to the patient’s medical record, she had unremarkable endocrine status and negative screening results for infections [toxoplasmosis, rubella cytomegalovirus, herpes simplex, HIV, syphilis, HBV (hepatitis B virus), and HCV (hepatitis C virus)]. The patient had a triple test (α-fetoprotein, human chorionic gonadotropin, and estriol) in her second trimester that showed low risk for Down syndrome. The fetus was sent for autopsy and developmental anomalies were excluded. Relevant laboratory values are shown in Table 1.
Questions to Consider
- How is recurrent pregnancy loss (RPL)4 defined and what is its frequency?
- List the most frequent causes of RPL.
- What diagnosis is suggested by the laboratory results?
Final Publication and Comments
The final published version with discussion and comments from the experts appears
in the May 2018 issue of Clinical Chemistry, approximately 3-4 weeks after the Student Discussion is posted.
Educational Centers
If you are associated with an educational center and would like to receive the cases and
questions 3-4 weeks in advance of publication, please email [email protected].
AACC is pleased to allow free reproduction and distribution of this Clinical Case
Study for personal or classroom discussion use. When photocopying, please make sure
the DOI and copyright notice appear on each copy.
DOI: 10.1373/clinchem.2017.274720
Copyright © 2018 American Association for Clinical Chemistry