Summary
DOI: 10.1373/clinchem.2016.267823
A 46-year-old man, originally from Iran, with no relevant medical history, was admitted with intermittent acute colic pain in the lower abdomen with nausea and vomiting over the past few weeks.
Student Discussion
Student Discussion Document (pdf)
Cilie C. van ‘t Klooster,* Jan J. Uil, Joep van der Leeuw, Elaine F. Eppens, and Susanne C. Marczinski
Ziekenhuis Gelderse Vallei, Ede, the Netherlands.
*Address correspondence to this author at: UMC Utrecht, Heidelberglaan 100, 3584 CX, Utrecht, the Netherlands. Fax 887-555-639; e-mail [email protected]
Case Description
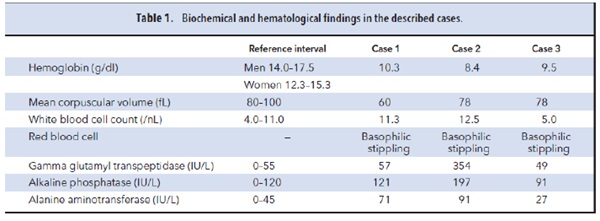
A 46-year-old man, originally from Iran, with no relevant medical history, was admitted with intermittent acute colic pain in the lower abdomen with nausea and vomiting over the past few weeks. On physical examination, the patient had lower abdominal pain without guarding. Laboratory findings showed a microcytic anemia, a heterozygote β-thalassemia, mild leukocytosis, and slight liver enzyme activity increase (Table 1, case 1). Hepatitis, cytomegalovirus, and Epstein–Barr virus were negative. Ultrasonography and computed tomography scan of the abdomen did not suggest liver, kidney, or pancreas disease, and gastroscopy and colonoscopy revealed no pathology. The patient denied substance abuse. The symptoms improved spontaneously and the patient awaited further diagnostics in the outpatient clinic. Within 1 week, the patient returned with similar symptoms. Acute intermittent porphyria (AIP)2 was suspected and urine porphyrins were measured. Urine δ-aminolevulinic acid (ALA) concentration was increased at 96.9 mmol/mol of creatinine (reference interval <3.9 mmol/mol creatinine), porphobilinogen (PBG) concentration was normal at 8 μmol/L (reference interval 0 –9 μmol/L), and coproporphyrinogen III concentration was increased at 91.8 nmol/mmol of creatinine (reference interval 2.9 –19.3 nmol/mmol of creatinine). These findings excluded the diagnosis AIP, as the PBG concentrations remained normal and both ALA concentration and coproporphyrinogen III concentrations increased.
Another 42-year-old man, originally from Iran and with no relevant medical history, presented with similar complaints of acute diffuse colic abdominal pain with nausea and vomiting. He complained of diffuse abdominal pain without guarding. Laboratory findings showed microcytic anemia, without signs of iron deficiency or thalassemia; basophilic stippling of red blood cells; mild leukocytosis; and increased liver enzyme activities (Table 1, case 2). Viral serology was negative. The patient denied substance abuse. Considering a gastric ulcer, a gastroscopy was performed that showed no abnormalities. Doppler ultrasonography of the abdomen was negative for liver, kidney, or pancreas disease, or mesenteric ischemia. On the basis of the symptoms, porphyrin analysis was performed, with the following results: ALA concentration was increased at 79.6 mmol/mol of creatinine and the free erythrocyte protoporphyrin concentration was also increased at 126.3 μg/dL (reference interval 0–65 μg/dL). The patient’s gums revealed Burton’s lines. Unknown
to the medical team at the time, the 2 patients were friends.
Soon after, a third patient, sibling of the aforementioned second case, presented with similar complaints, and the laboratory tests revealed similar results (Table 1,
case 3).
Questions to Consider
- What are the main causes of microcytic anemia?
- What are the diagnostic tests for acute intermittent porphyria?
- Which secondary porphyria can mimic acute porphyria?
Final Publication and Comments
The final published version with discussion and comments from the experts appears
in the December 2017 issue of Clinical Chemistry, approximately 3-4 weeks after the Student Discussion is posted.
Educational Centers
If you are associated with an educational center and would like to receive the cases and
questions 3-4 weeks in advance of publication, please email [email protected].
AACC is pleased to allow free reproduction and distribution of this Clinical Case
Study for personal or classroom discussion use. When photocopying, please make sure
the DOI and copyright notice appear on each copy.
DOI: 10.1373/clinchem.2016.267823
Copyright © 2017 American Association for Clinical Chemistry