Summary
DOI: 10.1373/clinchem.2016.258616
An 85-year-old man presented to his family physician with complaints of generalized weakness, fatigue, loss of appetite, excessive sleeping, and mild laryngitis. He reported that his temperature taken orally at home that morning was 102.6 °F. These symptoms arose during the previous week, before which he had been healthy, exercising vigorously every day.
Student Discussion
Student Discussion Document (pdf)
Jay L. Bock,* Lisa Senzel, Eric D. Spitzer, and William Bifulco
Stony Brook University, Stony Brook, NY.
*Address correspondence to this author at: Stony Brook University, Lab Administration Z-7300 Stony Brook University, Med. Ctr. 100 Nicolls Rd., Stony Brook, NY, 11794-7300. Fax 631-444-2653; e-mail [email protected].
Case Description
An 85-year-old man presented to his family physician with complaints of generalized weakness, fatigue, loss of appetite, excessive sleeping, and mild laryngitis. He reported that his temperature taken orally at home that morning was 102.6 °F. These symptoms arose during the previous week, before which he had been healthy, exercising vigorously every day. His past medical history included type 2 diabetes, hypercholesterolemia, and Paget disease of bone, and medications included metformin and pravastatin. One year earlier he had a tick bite followed
by appearance of a bullseye rash and took a course of doxycycline. He was not symptomatic after that and was not known to have any additional tick bites. He lived in Long Island, New York, and did not have a history of travel or sick contacts.
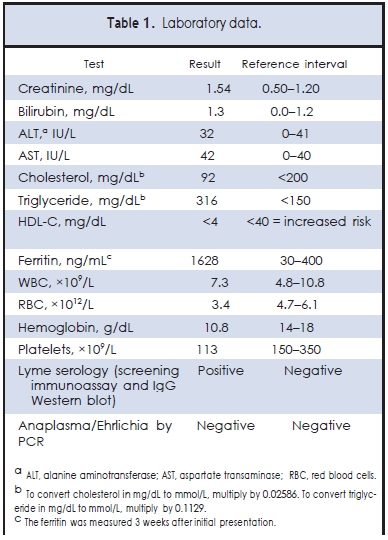
On physical exam the patient was alert but somewhat confused, with shaking chills. Cardiac and respiratory exam findings were normal. Laboratory testing included examination of a peripheral blood smear, which revealed intraerythrocytic ring forms, consistent with Babesia species, in 2.7% of the cells. The patient also had a lipid panel drawn (presumably because it was a visit to his family physician who ordered this as a routine) and was found to have an undetectable concentration of HDL cholesterol (HDL-C).2 Other laboratory data are summarized in Table 1.
The patient was diagnosed with babesiosis and admitted to the hospital, where he was treated with atovaquone, azithromycin, and doxycycline. Follow-up molecular testing confirmed infection with Babesia microti. Parasitemia declined to <0.1%, symptoms improved greatly, and he was discharged after 3 days. Ten weeks after initial presentation, anemia and thrombocytopenia had resolved. HDL-C had returned to a value within the reference interval (52 mg/dL or 1.34 mmol/L), and ferritin, which had been high, also was within the reference interval (293 ng/mL).
Questions to Consider
- What laboratory findings are characteristic of babesiosis?
- What conditions can cause markedly decreased HDL-C?
- What caused this patient to have a very marked, but transient, decrease in HDL-C?
Final Publication and Comments
The final published version with discussion and comments from the experts appears
in the March 2017 issue of Clinical Chemistry, approximately 3-4 weeks after the Student Discussion is posted.
Educational Centers
If you are associated with an educational center and would like to receive the cases and
questions 3-4 weeks in advance of publication, please email [email protected].
AACC is pleased to allow free reproduction and distribution of this Clinical Case
Study for personal or classroom discussion use. When photocopying, please make sure
the DOI and copyright notice appear on each copy.
DOI: 10.1373/clinchem.2016.258616
Copyright © 2017 American Association for Clinical Chemistry