Summary
DOI: 10.1373/clinchem.2016.264333
A 55-year-old woman was referred to the emergency department of Padova University Hospital with acute chest pain extending up to the left shoulder. She had had fever a few days prior but no other symptoms.
Student Discussion
Student Discussion Document (pdf)
Martina P. Marra,1 Martina Zaninotto,2 Luisa Cacciavillani,1 Sabino Iliceto,1 and Mario Plebani2*
1Department of Cardiac, Thoracic and Vascular Sciences, University of Padova, Italy; 2Department of Laboratory Medicine, University-Hospital, Padova, Italy.
*Address correspondence to this author at: Department of Laboratory Medicine, University-Hospital, via Giustiniani, 2, Padova 35128, Italy. Fax +39-049-663240; e-mail [email protected].
Case Description
A 55-year-old woman was referred to the emergency department of Padova University Hospital with acute chest pain extending up to the left shoulder. She had had fever a few days prior but no other symptoms. The patient, who was obese, smoked, and had a history of arterial hypertension, first received first-line amlodipine treatment that was interrupted because of poor compliance. No other traditional cardiovascular or thrombophilic risk factors were reported.
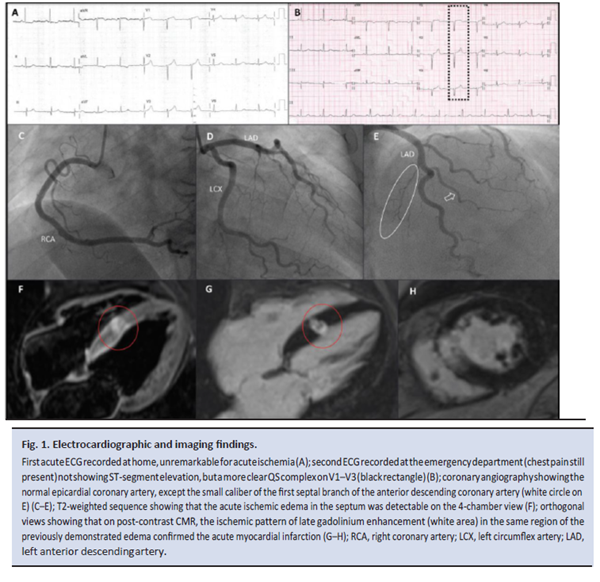
One hour after the onset of chest pain, the patient called the emergency service; the electrocardiogram (ECG)3 recorded at home was unremarkable for acute ischemia (Fig. 1A). At the emergency department, after 80 min, the patient still complained of chest pain, the physical examination was negative, blood pressure was 220/110 mmHg, and heart rate was 78 beats/min. The results of the second ECG were the same as those of the first (Fig. 1B).
The initial cardiac troponin I (cTnI) concentration, obtained using a high-sensitivity assay (1), was markedly increased (57 ng/L) relative to the sex-dependent 99th percentile (16 ng/L). The chest pain resolved with blood pressure normalization following intravenous nitrate administration. The patient had complained of chest pain for 100–120 min. An ECG performed after laboratory testing revealed normal left ventricular volumes and systolic function, with no cine wall motion abnormalities or other pathological signs. Contrast computerized tomography was conducted to rule out aortic dissection given the discrepancy between the type of symptoms and positive cTnI but negative ECG and echocardiogram. The examination was negative for acute aortic syndromes and
no calcium was identified at the level of the coronary arteries. The patient was then transferred to the intensive coronary care unit for monitoring. The cTnI concentration on a second sample drawn 6 h later was 4017 ng/L. Chest pain had decreased, with the patient describing it as “chest discomfort”. Coronary angiography revealed normal main coronary arteries (Fig. 1C–E), without cine wall motion abnormalities at left ventricular angiography; during the procedure, neither coronary vasospasm nor embolization were documented. The cTnI peak value was 22132 ng/L on the second day, with kinetics typical of acute coronary syndrome. Contrast-enhanced cardiac magnetic resonance (CE-CMR) imaging, performed on day 6 to rule out myocarditis, showed focal akinesia of the interventricular septum between the basal and mid segments; on T2-weighted sequence, a hyperintense signal intensity due to myocardial edema was present in the same region of cine abnormalities
(Fig. 1F). Finally, postcontrast T1-inversion recovery sequences evidenced transmural late
gadolinium enhancement with an ischemic pattern and an associated hypointense core
because of microvascular damage, thus indicating acute focal transmural myocardial
infarction of the interventricular septum (Fig. 1G–H). In view of the CE-CMR findings, the
coronary angiography was reevaluated and the small caliber of the first septal branch of the
anterior descending coronary artery was confirmed (Fig. 1E). The patient was discharged
on complete antiischemic and double antiplatelet drug therapy.
Reference
- Krintus M, Kozinski M, Boudry P, Capell NE, Köller U, Lackner K, et al. European multicenter analytical evaluation of the Abbott ARCHITECT STAT high sensitive troponin I immunoassay. Clin Chem Lab Med 2014;52:1657– 65.
Questions to Consider
- What are the causes of chest pain in adults with cardiovascular risk factors?
- What are the common causes of troponin release?
- What are the kinetics typical of troponin release in acute coronary syndrome?
Final Publication and Comments
The final published version with discussion and comments from the experts appears
in the March 2017 issue of Clinical Chemistry, approximately 3-4 weeks after the Student Discussion is posted.
Educational Centers
If you are associated with an educational center and would like to receive the cases and
questions 3-4 weeks in advance of publication, please email [email protected].
AACC is pleased to allow free reproduction and distribution of this Clinical Case
Study for personal or classroom discussion use. When photocopying, please make sure
the DOI and copyright notice appear on each copy.
DOI: 10.1373/Clinchem.2007.097139
Copyright © 2017 American Association for Clinical Chemistry