Summary
DOI: 10.1373/clinchem.2015.248039
A 35-year-old woman had thyroid function tests performed as part of a workup for infertility. Thyroid-stimulating hormone (TSH) was suppressed at 0.04 mIU/L (reference interval 0.45– 4.50) and free thyroxine (fT4) was 1.22 ng/dL [0.77–1.78 ng/dL (15.8 pmol/L, 10–23)]. Results were consistent with subclinical hyperthyroidism.
Student Discussion
Student Discussion Document (pdf)
Shao Feng Mok,1* E. Shyong Tai,1 Doddabele Srinivasa Deepak,1 and Tze Ping Loh2
Departments of 1Medicine and 2Laboratory Medicine, National University Hospital, Singapore.
*Address correspondence to this author at: National University Hospital, 5 Lower Kent Ridge Rd., Singapore 119074. Fax +65 67771613; e-mail [email protected].
Case Description
A 35-year-old woman had thyroid function tests performed as part of a workup for infertility. Thyroid-stimulating hormone (TSH) was suppressed at 0.04 mIU/L (reference interval 0.45– 4.50) and free thyroxine (fT4) was 1.22 ng/dL [0.77–1.78 ng/dL (15.8 pmol/L, 10–23)]. Results were consistent with subclinical hyperthyroidism.
Five months later, TSH was markedly increased (28.6 mIU/L) while fT4 remained within the reference interval (0.92 ng/dL). Antithyroid peroxidase antibodies (TPOAb) were negative (˂40 IU/mL), and TSH receptor autoantibodies (TRAb) were markedly increased at 40 IU/L (˂1.8 IU/L). The patient denied any symptoms apart from her infertility.
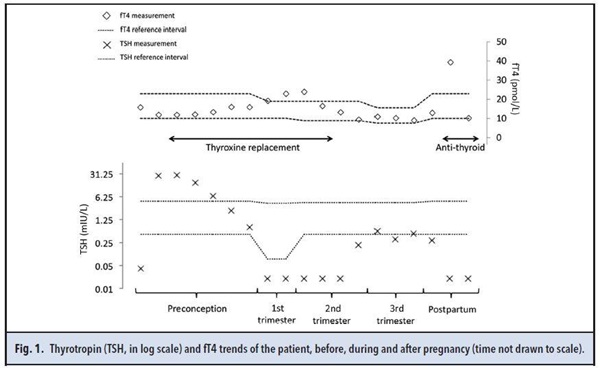
Based on clinical and laboratory features, the diagnosis of blocking TRAb-related subclinical hypothyroidism (SCH) with infertility was made. The patient was started on thyroxine replacement to reduce TSH to ˂2.5 mIU/L before in vitro fertilization. She achieved the TSH target 6 month later and conceived successfully after 3 cycles of in vitro fertilization. During pregnancy, her TSH was suppressed, with fT4 within or slightly above the reference interval despite gradual reduction and discontinuation of thyroxine replacement. TSH suppression due to high human chorionic gonadotropin (hCG) concentration in pregnancy usually wanes in the second trimester when hCG concentrations fall. Therefore, this patient’s persistent TSH suppression could not be solely accounted for by the effects of hCG (Fig. 1). The patient remained clinically euthyroid throughout the pregnancy. She delivered a healthy boy via a normal vaginal delivery at 39 weeks of gestation. Postpartum, serial monitoring of TSH showed persistent suppression for up to 6 months while the fT4 gradually increased. At this time, her clinical features suggested the development of hyperthyroidism (Fig. 1).
Questions to Consider
- How is SCH defined?
- What are the subtypes of TRAb and what laboratory assays are used to detect and distinguish between them?
- What could explain this patient’s changes in thyroid hormone testing results and clinical symptoms?
Final Publication and Comments
The final published version with discussion and comments from the experts appears
in the October 2016 issue of Clinical Chemistry, approximately 3-4 weeks after the Student Discussion is posted.
Educational Centers
If you are associated with an educational center and would like to receive the cases and
questions 3-4 weeks in advance of publication, please email [email protected].
AACC is pleased to allow free reproduction and distribution of this Clinical Case
Study for personal or classroom discussion use. When photocopying, please make sure
the DOI and copyright notice appear on each copy.
DOI: 10.1373/clinchem.2015.248039
Copyright © 2016 American Association for Clinical Chemistry