Summary
DOI: 10.1373/clinchem.2014.234849
An 18-year-old woman presented with persistent bilateral lactation, excess body weight, and recurrent hypercalcemia. At age 13 years, before menarche, she developed bilateral milk discharge from her breasts.
Student Discussion
Student Discussion Document (pdf)
Qing H. Meng,1* and Elizabeth A. Wagar1
1Department of Laboratory Medicine, The University of Texas MD Anderson Cancer Center, Houston, TX.
*Address correspondence to this author at: Department of Laboratory Medicine, The University of Texas MD Anderson Cancer Center, 1515 Holcombe Blvd., Unit 37, Houston, TX 77030-4009. Fax +713-792-4793; E-mail [email protected].
Case Description
An 18-year-old woman presented with persistent bilateral lactation, excess body weight, and recurrent hypercalcemia. At age 13 years, before menarche, she developed bilateral milk discharge from her breasts. The lactation continued and, at age 16 years, she experienced
increasingly frequent headaches and visual field changes; her prolactin concentration was noted to be >2400 ng/mL. A year later, she underwent transsphenoidal resection of a pituitary macroadenoma. After the surgery, she developed panhypopituitarism and central diabetes insipidus (DI). She was treated with levothyroxine (T4) for secondary hypothyroidism and received other hormone replacement therapy, including desmopressin acetate [a synthetic analog of antidiuretic hormone (ADH)], conjugated estrogen (Premarin), growth hormone (Humatrope), and bromocriptine. A year later, she developed recurrent kidney stones and was diagnosed with primary hyperparathyroidism. She was also found to have multiple thyroid nodules. She underwent a 4-gland parathyroidectomy with left forearm autograft and total thyroidectomy.
She had had transient hypoparathyroidism following parathyroidectomy, soon afterward she experienced recurrent primary hyperparathyroidism with nephrocalcinosis and pyelonephritis.
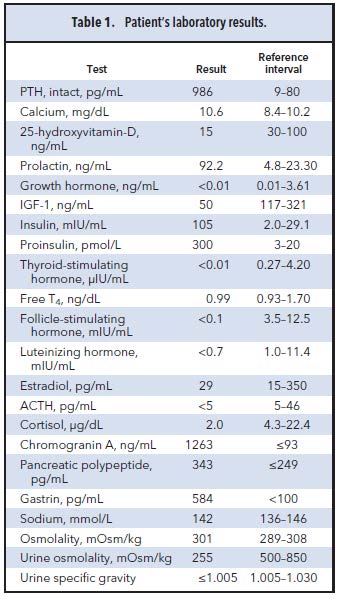
She came to our hospital to seek further evaluation and treatment. She had continued to gain weight and had developed depression and anxiety. She also reported joint pain, fatigue, blurry vision, loss of appetite, dyspnea, polyuria, and insomnia. She reported occasional diarrhea but no significant flatulence. There was no pertinent family history of endocrine disorders. Physical examination revealed an obese young woman in distress, with leg swelling and unbalanced gait. Her pulse was 91 beats per minute and blood pressure was 113/67 mmHg. Findings of the cardiovascular and respiratory examination were unremarkable. Multiple skin tags and nodules were noted over the trunk and abdomen and around her vaginal and groin region. The evaluation at our institution included laboratory investigations (Table 1), imaging, and histologic studies. An adrenocorticotropic hormone (ACTH) stimulation test (1 μg cosyntropin) showed a peak cortisol concentration of 18.7 μg/dL (reference interval >20 μg/dL). Complete blood cell count showed
microcytic hypochromic anemia.
Questions to Consider
- What diagnosis does this constellation of laboratory results and clinical symptoms suggest?
- What other disorders may be seen with this primary disease?
- What genetic testing would be indicated?
Final Publication and Comments
The final published version with discussion and comments from the experts appears
in the November 2015 issue of Clinical Chemistry, approximately 3-4 weeks after the Student Discussion is posted.
Educational Centers
If you are associated with an educational center and would like to receive the cases and
questions 3-4 weeks in advance of publication, please email [email protected].
AACC is pleased to allow free reproduction and distribution of this Clinical Case
Study for personal or classroom discussion use. When photocopying, please make sure
the DOI and copyright notice appear on each copy.
DOI: 10.1373/clinchem.2014.234849
Copyright © 2015 American Association for Clinical Chemistry