Summary
DOI: 10.1373/clinchem.2012.194720
A previously healthy 4-year-old girl presented with a 2-day history of severe nausea, vomiting, and diarrhea. Her symptoms began with diffuse abdominal pain followed by alternating episodes of vomiting and nonbloody diarrhea. There were no reports of sick contacts, recent travel, camping, or unusual food or water consumption.
Student Discussion
Student Discussion Document (pdf)
Kristina N. Carswell,1 Wafi Bibars,2 Saad Mir,3 Neil Harris,2 and Michele N. Lossius1*
1 Department of Pediatrics and 2 Department of Pathology, Immunology, and Laboratory Medicine, University of Florida College of Medicine, Gainesville, FL; 3 University of Florida College of Medicine, Gainesville, FL.
* Address correspondence to this author at: P.O. Box 100296, Gainesville, FL 32610. Fax 352-276-5265; E-mail: [email protected].
Case Description
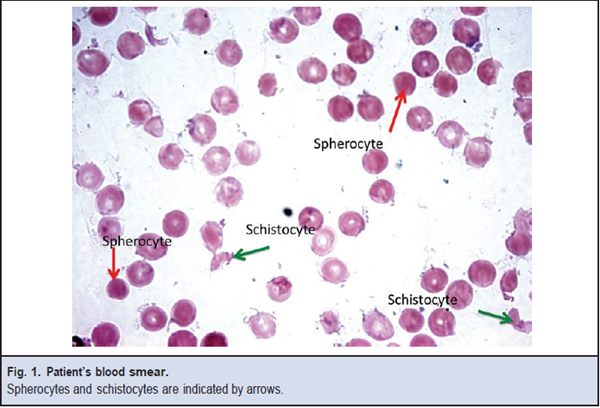
A previously healthy 4-year-old girl presented with a 2-day history of severe nausea, vomiting, and diarrhea. Her symptoms began with diffuse abdominal pain followed by alternating episodes of vomiting and nonbloody diarrhea. There were no reports of sick contacts, recent travel, camping, or unusual food or water consumption. On the first day of symptoms, her primary care physician diagnosed viral gastroenteritis and stool cultures were sent to an outside laboratory. The following day, her vomiting increased in frequency and the diarrhea became streaked with blood and mucus. The patient was taken to a regional hospital where a complete blood count revealed a white blood cell count of 22 500/mL (reference interval, 5.5–15.5 × 1000/mL) with 89% neutrophils and 7% bands. A urinalysis revealed positive ketones of 150 mg/dL (reference value, negative) and a specific gravity of 1.030 (reference interval, 1.005–1.030). She was then transferred to our hospital for management of neutrophilia and dehydration. On admission, her temperature was 38.7 °C, but other vital signs and physical exam results were unremarkable. She was treated with intravenous fluids. Stool cultures for bacteria, shiga toxin, ova, and parasites were obtained. Urinalysis showed positive protein of 300 mg/dL protein (reference value, negative) and 4 red blood cells per high-power field (reference value, negative). On day 2 of admission, the patient passed cranberry-colored urine. Repeat laboratory test results at this time revealed creatinine of 1.10 mg/dL (97.2 μmol/L) (reference interval, 0.03–0.7 mg/dL), a blood urea nitrogen (BUN) of 26 mg/dL (9.3 mmol/L) (reference interval, 6–20 mg/dL), a hematocrit of 30.7% (reference interval, 34.0%–40.0%), and a platelet count of 28 000/mL (reference interval, 150–450 × 1000/mL). Her blood smear is shown in Fig. 1. She continued to demonstrate anemia and thrombocytopenia throughout her hospital admission. Her stool cultures (and blood cultures) sent on admission were negative for pathogens.
Questions to Consider
- What diagnosis is most likely in light of the clinical presentation?
- What laboratory tests or radiologic imaging is/are required to make the appropriate diagnosis?
- What organisms are typically implicated in this disease?
- What is the expected clinical course of this disease?
Final Publication and Comments
The final published version with discussion and comments from the experts appears
in the September 2013 issue of Clinical Chemistry, approximately 3-4 weeks after the Student Discussion is posted.
Educational Centers
If you are associated with an educational center and would like to receive the cases and
questions 3-4 weeks in advance of publication, please email [email protected].
AACC is pleased to allow free reproduction and distribution of this Clinical Case
Study for personal or classroom discussion use. When photocopying, please make sure
the DOI and copyright notice appear on each copy.
DOI: 10.1373/clinchem.2012.194720
Copyright © 2013 American Association for Clinical Chemistry