Summary
DOI: 10.1373/clinchem.2012.188409
A 3-year-old girl presented with petechial hemorrhages and repeated nosebleeds. Two weeks earlier she had been admitted to a local hospital with nosebleeds accompanied by 2 episodes of vomiting dark red blood. Results of the laboratory evaluation included: white blood cell count, 8.2 × 109/L [reference interval (RI),3 4 × 109/L to 10 × 109/L]; hemoglobin, 10.7 g/dL (RI, 11–15 g/dL); platelet count, 142 × 109/L (RI, 100 × 109/L to 300 × 109/L), prothrombin time, 11.5 s (RI, 9–13 s); activated partial thromboplastin time, 31.2 s (RI, 26–39 s); and fibrinogen, 2.5 g/L (RI, 2.0–4.0 g/L). The patient was discharged in good condition after insertion of nasal packs.
Student Discussion
Student Discussion Document (pdf)
Peipei Jin,1 Lijun Qiu,1 Siguo Hao,2 Xiangliang Yuan,1 and Lisong Shen1*
1Departments of Clinical Laboratory and 2Hematology, Xinhua Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China.
*Xin Hua Hospital, 1665 Kong Jiang Rd., Yangpu District, Shanghai, NA, China 200092. Fax: 21-25075173;
E-mail: [email protected].
Case Description
A 3-year-old girl presented with petechial hemorrhages and repeated nosebleeds. Two weeks earlier she had been admitted to a local hospital with nosebleeds accompanied
by 2 episodes of vomiting dark red blood. Results of the laboratory evaluation included: white blood cell count, 8.2 × 109/L [reference interval (RI), 4 × 109/L to 10 × 109/L]; hemoglobin, 10.7 g/dL (RI, 11–15 g/dL); platelet count, 142 × 109/L (RI, 100 × 109/L to 300 × 109/L), prothrombin time, 11.5 s (RI, 9–13 s); activated partial thromboplastin time, 31.2 s (RI, 26–39 s); and fibrinogen, 2.5 g/L (RI, 2.0–4.0 g/L). The patient was discharged in good condition after insertion of nasal packs.
One day before the current admission, the patient had nose bleeds once again, this time accompanied by 4 episodes of hematemesis and tarry stool. At presentation, she had no fever and no diarrhea. She was not on any medications. The patient had a history of easy bruising, repeated gum bleeding, but not hemarthrosis. There was no family history of abnormal bleeding. On examination, she appeared pale, with normal vital signs. Her skin had scattered petechiae. The physical examination was otherwise unremarkable.
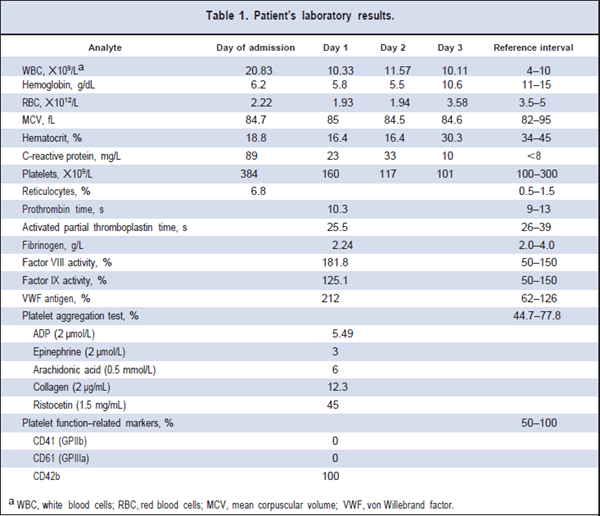
At presentation, laboratory findings included the following: hemoglobin, 6.2 g/dL (RI, 11–15 g/dL); reticulocyte count, 6.8% (RI, 0.5%–1.5%). Other laboratory results are shown in Table 1.
In vitro testing showed that the patient’s platelets did not aggregate in response to ADP, epinephrine, arachidonic acid, or collagen, but platelets had relatively normal ristocetin-induced aggregation. These findings were confirmed on repeat testing. A smear of peripheral blood showed no clusters of normal platelets. A flow cytometry evaluation revealed marked reduction in glycoprotein IIb/IIIa (GPIIb/IIIa).
Questions to Consider
- What disorders should be considered in the workup of children with repeated nose bleeds?
- What are the potential sources of preanalytical variation in hematologic tests?
- What is the most likely cause of the results seen in this case?
- What are the typical symptoms and laboratory test results associated with various inherited causes of platelet dysfunction?
Final Publication and Comments
The final published version with discussion and comments from the experts appears
in the May 2013 issue of Clinical Chemistry, approximately 3-4 weeks after the Student Discussion is posted.
Educational Centers
If you are associated with an educational center and would like to receive the cases and
questions 3-4 weeks in advance of publication, please email [email protected].
AACC is pleased to allow free reproduction and distribution of this Clinical Case
Study for personal or classroom discussion use. When photocopying, please make sure
the DOI and copyright notice appear on each copy.
DOI: 10.1373/clinchem.2012.188409
Copyright © 2013 American Association for Clinical Chemistry