Summary
DOI: 10.1373/clinchem.2013.204438
A 60-year-old man presented to his general practitioner with complaints of indigestion and flu-like symptoms. The results of a clinical examination were unremarkable. The only abnormality found in routine hematology and biochemistry investigations was an increased serum alkaline phosphatase concentration (131 U/L; reference interval, 35–120 U/L).
Student Discussion
Student Discussion Document (pdf)
Andrew S. Davison,1* Stewart J. Pattman,2 Robert D.G. Neely,2 Richard Bliss,3 and Steve G. Ball4,5
1Department of Clinical Biochemistry, Royal Liverpool and Broadgreen University Hospitals Trust, Liverpool, UK; Departments of 2Clinical Biochemistry, 3Surgery, and 4 Endocrinology, Royal Victoria Infirmary, Newcastle upon Tyne NHS Foundation Trust, Newcastle upon Tyne, UK; 5School of Medical Sciences Education Development, Medical School, University of Newcastle, Newcastle, UK.
*Department of Clinical Biochemistry, Royal Liverpool and Broadgreen University Hospitals Trust, Liverpool L7 8XP,
UK. Fax +0151-706-4250; E-mail [email protected].
Case Description
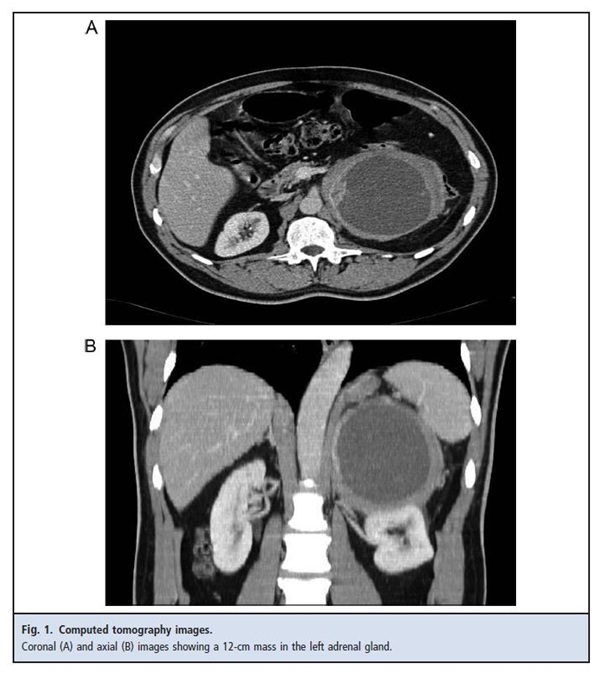
A 60-year-old man presented to his general practitioner with complaints of indigestion and flu-like symptoms. The results of a clinical examination were unremarkable. The only abnormality found in routine hematology and biochemistry investigations was an increased serum alkaline phosphatase concentration (131 U/L; reference interval, 35–120 U/L). Given his abdominal discomfort, the patient was referred for an abdominal ultrasound evaluation, which revealed a 12-cm cystic mass in the area of the left kidney. Further imaging with computed tomography scanning suggested that the mass arose from the left adrenal gland (Fig. 1). The patient’s medical history was notable for hypertension, which was controlled with 8 mg candesartan once daily. The patient reported no headaches, palpitations, or diaphoresis.
The patient was referred for further investigation. Plasma free metanephrines (PMets) were measured. Initial results showed borderline increases in plasma normetanephrine (NMN) and metanephrine (MN) that were not diagnostic of pheochromocytoma (PCC). PMet measurements were repeated with a separate plasma sample, and total fractionated urine MNs (UMets) were measured in a sample of an acidified 24-h urine collection. Urine and plasma analysis results were concordant, with borderline increases in NMN
(Table 1). The patient was not on any medications known to cause a physiological increase in PMets.
Case Follow-Up
On the basis these findings, the size of the mass, and the lack of interfering medications, the patient underwent α-blockade with 10 mg phenoxybenzamine 3 times per day and surgical resection of the adrenal mass. A subsequent histologic analysis revealed a cystic PCC with evidence of intratumoral hemorrhage and degeneration. PMet concentrations returned to normal after tumor resection (Table 1). Subsequent testing identified no germline mutations in PCC-predisposing genes, a result consistent with sporadic disease. During follow-up the patient remained normotensive and off antihypertensive medication.
Questions to Consider
- How should borderline increases in MNs be interpreted and followed up?
- How best should one integrate clinical, radiologic, and biochemical features of adrenal masses?
- How do sampling conditions and medications affect MN and NMN concentrations?
Final Publication and Comments
The final published version with discussion and comments from the experts appears
in the November 2013 issue of Clinical Chemistry, approximately 3-4 weeks after the Student Discussion is posted.
Educational Centers
If you are associated with an educational center and would like to receive the cases and
questions 3-4 weeks in advance of publication, please email [email protected].
AACC is pleased to allow free reproduction and distribution of this Clinical Case
Study for personal or classroom discussion use. When photocopying, please make sure
the DOI and copyright notice appear on each copy.
DOI: 10.1373/clinchem.2013.204438
Copyright © 2013 American Association for Clinical Chemistry