Summary
DOI: 10.1373/clinchem.2010.156364
A 57-year-old man developed numbness and tingling in his toes, which progressed over 3 to 4 months to involve his legs, hands, and lower torso. He then developed trouble walking owing to imbalance and had increasingly frequent falls. His hands felt clumsy, and he began dropping objects. He reported several instances of urinary incontinence in the weeks before presentation, but no bowel symptoms. He denied focal weakness or changes in speech, swallowing, or breathing. His sisters brought him to the emergency room after a fall in which he hit his head on a kitchen stool, and he was admitted to the neurology service for further evaluation.
Student Discussion
Student Discussion Document (pdf)
R. Brian Sommerville,1* and Robert H. Baloh1,2*
1Department of Neurology, Neuromuscular Division, and 2Hope Center for Neurological Disorders, Washington University School of Medicine, St. Louis, MO.
*Address correspondence to: R.B.S. at Department of Neurology, Washington University School of Medicine, 660 S. Euclid Ave., Box 8111, St. Louis, MO 63110. E-mail [email protected]. R.H.B. at Department of Neurology, Washington University School of Medicine, 660 S. Euclid Ave., Box 8111, St. Louis, MO 63110. E-mail [email protected]
Case Description
A 57-year-old man developed numbness and tingling in his toes, which progressed over 3 to 4 months to involve his legs, hands, and lower torso. He then developed trouble walking owing to imbalance and had increasingly frequent falls. His hands felt clumsy, and he began dropping objects. He reported several instances of urinary incontinence in the weeks before presentation, but no bowel symptoms. He denied focal weakness or changes in speech, swallowing, or breathing. His sisters brought him to the emergency room after a fall in which he hit his head on a kitchen stool, and he was admitted to the neurology service for further evaluation.
The patient’s medical history included longstanding tobacco use, chronic obstructive pulmonary disease, and low back pain. In addition, 5 months before the onset of his paresthesias, he was discovered to have a macrocytic anemia that did not respond to treatment with vitamin B12 and folate. He was subsequently treated with periodic blood transfusions.
The general physical examination was unremarkable. On neurologic examination, the patient’s mental status and cranial nerves were normal. A motor examination revealed spasticity without weakness in the legs. There was severe loss of vibratory and joint position sensation in the upper and lower extremities in a stocking-glove distribution; pain and temperature sensation were relatively spared. Reflexes were normal to brisk throughout, and there was no extensor toe sign. Finger tapping and toe tapping were mildly slowed. The Romberg sign was present. The patient’s gait was slow, stiff-appearing, and ataxic, with a widened base and marked truncal instability. The constellation of lower extremity–predominant spasticity and proprioceptive defects suggested an abnormality in the region of the cervical spinal cord.
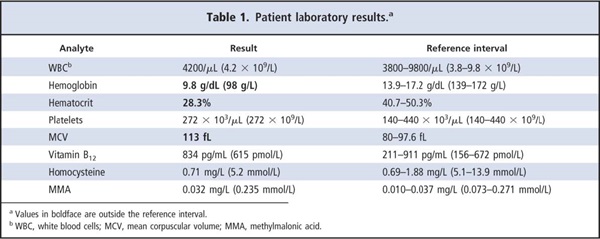
A laboratory workup on the patient’s admission revealed macrocytic anemia (Table 1). The vitamin B12 concentration was in the upper part of the reference interval, and the concentrations of cobalamin pathway metabolites homocysteine and methylmalonic acid were within reference intervals. Despite the normal B12 concentration, B12 repletion was instituted, but symptoms did not improve. An MRI evaluation of the spinal cord excluded compression but identified abnormal T2 signal along the posterior regions of the cervical and upper thoracic cord. Nerve-conduction studies showed a mild sensory peripheral neuropathy. Further questioning revealed that the patient had worn dentures for 10 years and that family members frequently chided him for excessive use of denture adhesive to the extent that it sometimes accumulated at the corners of his mouth.
Questions to Consider
- What is in the differential diagnosis of a noncompressive myelopathy?
- What are some causes of macrocytic anemia?
- Could the excessive use of dental adhesive contribute to the patient’s symptoms?
Final Publication and Comments
The final published version with discussion and comments from the experts appears
in the August 2011 issue of Clinical Chemistry, approximately 3-4 weeks after the Student Discussion is posted.
Educational Centers
If you are associated with an educational center and would like to receive the cases and
questions 3-4 weeks in advance of publication, please email [email protected].
AACC is pleased to allow free reproduction and distribution of this Clinical Case
Study for personal or classroom discussion use. When photocopying, please make sure
the DOI and copyright notice appear on each copy.
DOI: 10.1373/clinchem.2010.156364
Copyright © 2011 American Association for Clinical Chemistry