 The convenience and immediacy of point-of-care testing (POCT) has led to its use in many settings. But untrained or busy healthcare workers may overlook some basic sanitary practices when using POCT devices. This lack of attention is leading to nosocomial infections that can be attributed to contaminated devices. Here, Sharon M. Geaghan, MD, discusses how these infections occur and how to prevent them. Dr. Geaghan is professor of pathology and pediatrics at Stanford University School of Medicine in Palo Alto, Calif.
The convenience and immediacy of point-of-care testing (POCT) has led to its use in many settings. But untrained or busy healthcare workers may overlook some basic sanitary practices when using POCT devices. This lack of attention is leading to nosocomial infections that can be attributed to contaminated devices. Here, Sharon M. Geaghan, MD, discusses how these infections occur and how to prevent them. Dr. Geaghan is professor of pathology and pediatrics at Stanford University School of Medicine in Palo Alto, Calif.
Michael Astion, MD, PhD, chair of the Patient Safety Focus Editorial Advisory Board, conducted this interview.
How would you sum up the problem related to POCT and nosocomial infections?
Overall, I would say that there is a significant and pervasive lack of awareness about nosocomial infections associated with POCT, especially hepatitis B infections.
In what settings do these infections occur?
Typically, these infections occur during assisted monitoring of a POCT analyte. By assisted monitoring, I mean a POCT procedure performed by a nurse or other healthcare provider for the patient, rather than by the patient. Frequently, this involves a diabetic patient who is being helped with monitoring his or her blood glucose; however, any POCT device can transmit infection. These infections have been found in a variety of health care settings, including hospitals, ambulatory surgery centers, outpatient clinics, and assisted living facilities.
What infectious agents are most likely to be transmitted by POCT devices?
Hepatitis B and C are the most likely, although any blood-borne pathogen can be transmitted. For example, in one assisted living facility in North Carolina, officials discovered unsafe POCT practices that had significant consequences. Eight of 15 patients who had assisted POCT glucose monitoring contracted hepatitis B, and six died from the infection. While the severity of any infection transmitted in this manner can vary, this example illustrates that patients can suffer dire outcomes from POCT-transmitted nosocomial infections.
How are these infections transmitted?
There are several mechanisms, such as using a multi-lancet, finger-stick device on more than one patient; inadequately disinfecting and cleaning the POCT device between patients; placing meters in contaminated storage areas; and failing to change gloves and thoroughly wash hands between patients. It's important to note that the highest risk for inadequate hand hygiene and glucose meter disinfection occurs when healthcare workers must assist large numbers of patients and only a few devices are available.
As laboratorians know, POCT devices frequently become contaminated with blood. What many healthcare workers fail to recognize, however, is that transmission of infectious agents can occur even if no blood is visible on the finger-stick or POCT device.

Healthcare professionals need to take extra precautions in assisted living facilities
to prevent transmitting infections from contaminated POCT devices.
Do glucose meters have to be cleaned and disinfected after every use?
Yes, especially if the meter is being used sequentially on different patients. In assisted living facilities, patients usually have dedicated meters. Even so, proper storage of the device is still important. It's best to store the meter in the patient's room, so that the risk of accidentally using the device on another patient and cross-contamination by contact with a blood-contaminated storage area or other equipment is eliminated. If the meter is reassigned to another patient, then it must be cleaned and disinfected.
Healthcare workers may not be aware that meters can become contaminated in unsanitary storage areas. Even if the meter does not come in direct contact with patients, indirect transmission can occur via healthcare workers who handled the contaminated device. It's also important to note that many institutions use alcohol wipes to disinfect devices. These wipes are not effective against hepatitis B virus present in dried blood. Instead, devices should be cleaned and disinfected with bleach-based disinfectants that are effective against hepatitis B and C.
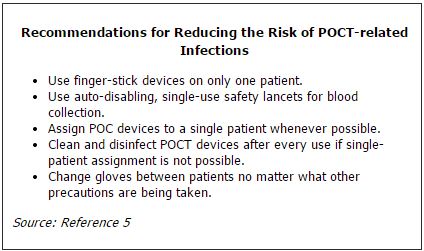
Can you summarize the recommendations to reduce the risk of POCT-related infections?
The Food and Drug Administration and the Centers for Disease Control and Prevention have made some recommendations (See Table). The recommendations focus on cleaning and disinfecting instruments, proper hand hygiene, and implementing single-use finger-stick devices whenever possible. Assigning POCT instruments to a single patient is recommended as a best practice.
REFERENCES
- Louie RF, Lau MJ, Lee JH, et al. Multicenter study of the prevalence of blood contamination on point of care glucose meters and recommendations for controlling contamination. Point Care 2005;4:158–63.
- CDC. Notes from the field: deaths from acute hepatitis B virus infection associated with assisted blood glucose monitoring in an assisted living facility—North Carolina, August–October 2010. MMWR Morb Mortal Wkly Rep 2011;60:182.
- CDC. Multiple outbreaks of hepatitis B virus infection related to assisted monitoring of blood glucose among residents of assisted living facilities—Virginia, 2009–2011. MMWR Morb Mortal Wkly Rep 2012;61:339–43.
- Thompson ND, Schaefer MK. "Never Events": hepatitis B outbreaks and patient notifications resulting from unsafe practices during assisted monitoring of blood glucose, 2009–2010. J Diabetes Sci Technol 2011;5:1396–402.
- FDA Patient Safety News. Preventing infections while monitoring glucose. Available online. (Accessed November 2012).