
The incidence of kidney stones, an extremely painful urologic disorder associated with significant morbidity, has been increasing in the U.S. during the past 30 years. Today, up to 12% of men and 5% of women will develop at least one kidney stone by age 70. Recurrence rates are estimated to be as high as 50%, giving credence to the old adage "once a stone former, always a stone former." Furthermore, the disease creates a large economic burden on the U.S. healthcare system, with a total estimated cost of $5.3 billion annually.
Kidney stones can form when urine contains too much of certain substances. These substances create small crystals that may go on to form stones over the course of weeks or months. Laboratory evaluation of kidney stones not only helps in identifying the constituents of the stone, but also in determining the underlying cause of stone formation, knowledge that is helpful for preventing stone recurrence. This article describes metabolic conditions that contribute to stone formation, as well as the laboratory tests used to evaluate patients.
Pathogenesis of Kidney Stones
Various factors contribute to the formation of kidney stones. Supersaturation of urine by constituents, such as cystine, calcium, or oxalate, is the most widely accepted mechanism for stone formation. Normally, when the solute concentration reaches the saturation point and crystallization begins, it is impeded by inhibitors present in urine, including citrate, pyrophosphate, glycosaminoglycans, nephrocalcin, and Tamm-Horsfall protein. As solute concentration continues to increase, however, a critical supersaturation point is reached. Above this level, inhibitors of crystallization become ineffective and spontaneous crystallization can occur.
Types of Stones
There are four major classifications of kidney stones (Table 1). The most common type contains calcium. Struvite stones contain magnesium, ammonia, and phosphate. Other less common ones are composed of uric acid and cystine. Kidney stones may be as small as a grain of sand or as large as a pea. Some stones are even as big as golf balls. Stones may be smooth or jagged, and they usually are yellow or brown.
Calcium Stones
A majority of calcium stones consist of >90% oxalate with trace amounts of phosphate. Several factors contribute to formation of this type of stone. An estimated 40–60% of all calcium stone formers have hypercalciuria, which is either idiopathic or secondary to conditions that increase calcium excretion in urine, including primary hyperparathyroidism, vitamin D toxicity, and sarcoidosis. Idiopathic hypercalciuria, with a prevalence rate ranging from 2.9–6.5%, is defined as increased urinary calcium excretion in patients with an unrestricted calcium diet and no evidence of secondary causes.
There are three types of hypercalciuria: absorptive, caused by increased absorption of calcium in the jejunum; resorptive, caused by increased bone demineralization and turnover; and renal, caused by a primary defect in renal tubular calcium excretion. All three can co-exist and contribute to each other.
Calcium stones occur primarily in individuals who excrete excess levels of oxalate in urine. Hyperoxaluria arises from either increased oxalate absorption from the gut or increased dietary intake of oxalate. Because calcium binds with oxalate in the gut and hinders its absorption, oxalate is more readily absorbed when dietary calcium is low. Besides decreased dietary calcium intake, hyperoxaluria can be due to unusually high intake of oxalate-rich food products such as spinach, rhubarb, and nuts.
Enteric hyperoxaluria is a consequence of fat malabsorption, such as that seen in inflammatory bowel diseases or short bowel syndrome. In malabsorption, increased amounts of intraluminal fat and bile salt bind readily with calcium, leaving excess oxalate to be reabsorbed and excreted in the urine. In addition, bile salts and fat also increase colonic absorption of oxalate.
Primary hyperoxaluria, a rare autosomal recessive condition, causes disturbances in the oxalate biosynthetic pathway, leading to very high oxalate excretion.
An estimated 20–60% of calcium stone formers have reduced citrate excretion, leading to excess citrate. The citrate buildup reduces calcium oxalate super-saturation in urine by forming complexes with calcium and directly inhibiting crystal growth and aggregation. Researchers also have demonstrated that alkaline citrate therapy increases the clearance rate of residual stone fragments following extracorporeal shock-wave lithotripsy (ESWL). This treatment also reduces post-ESWL recurrence rates both in stone-free patients and those with residual fragments. More recently, evidence suggests that citrate has beneficial effects in normocitraturic stone formers. Researchers found that keeping citrate concentrations above the normal reference range was highly effective at inhibiting residual fragment growth. Intracellular renal tubular acidosis promotes proximal renal tubular reabsorption of citrate and reduces the citrate excretion, whereas alkalosis increases citrate excretion in urine.
Familial or acquired distal renal tubular acidosis (dRTA) is a condition in which the kidneys lose their ability to produce urine with a pH ≤5.5. It is usually accompanied by hypocitraturia, which precipitates the formation of calcium oxalate stones.
Calcium Phosphate Stones
Hypercalciuria and alkaline urine lead to formation of calcium phosphate stones. Patients with these types of stones have a significantly lower threshold of renal phosphate reabsorption. The ensuing hypophosphatemia stimulates calcitriol synthesis, resulting in hypercalciuria. Researchers believe that phosphaturia is due to defects in the sodium-phosphate transporter found in the proximal renal tubule. This defect contributes to increased concentration of both calcium and phosphate in the renal loop of Henle and creates conditions that favor stone formation.
Uric Acid Stones
Uric acid (UA) is an end product of purine metabolism that the body excretes in urine. Both purine overproduction and excess purine ingestion favor formation of UA stones. The three major risk factors for UA stones are low urine pH (<5.5), low urine volume, and hyperuricosuria. These factors result in undissociated UA, a poorly soluble molecule that contributes to precipitation and crystallization. As pH rises, it dissociates into a more soluble urate ion.
Patients without any obvious underlying congenital or acquired conditions are known as idiopathic UA stone formers. In these individuals, low urinary pH may be due to a defect in renal ammonium excretion that reduces the buffer for H+ and results in a pH increase. Some studies have suggested a link between this defect and insulin resistance.
Struvite Stones
Struvite stones consist of a mixture of magnesium, ammonium, and phosphate. They are associated with chronic urinary tract infections and are more prevalent in women. Several urea-splitting microorganisms are responsible for struvite stone formation, including Proteus, Staphylococcus, Klebsiella, and Pseudomonas. These bacteria hydrolyze urea to produce NH4+ and OH– ions that contribute to the alkalinity of urine. Both ammonium and alkaline urine are essential for struvite supersaturation of urine.
Cystine Stones
Cystinuria is an inheritable autosomal recessive disorder of amino acids transport, specifically cystine, arginine, ornithine, and lysine, that affects epithelial cells of the renal tubules and gastrointestinal tract. Researchers have identified mutations in two genes, SLC3A1 and SLC7A9, that encode defective subunits of the cystine transporter and that are responsible for most cases of cystinuria. Individuals with these mutations excrete increased amounts of urinary cystine. Because cystine has limited solubility, increased levels in urine favor its precipitation and contribute to formation of cystine stones. Stone formation usually is the only clinical manifestation of this disorder, which can occur at any age, although the mean is 20–40 years.
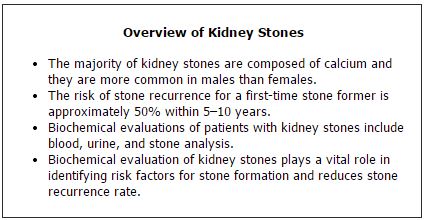
Biochemical Investigations of Risk Factors
Biochemical investigations help identify risk factors associated with stone formation, and help clinicians determine the most appropriate treatment and monitor its effectiveness. The goal of such efforts is to prevent stone recurrence. Analyses involve three components: blood, urine, and the actual stone.
Blood investigations assess levels of electrolytes, calcium, phosphate, uric acid, and parathyroid hormone, as well as renal and thyroid functions and vitamin D status.
Analysis of urine is probably the most important element of assessing patients, irrespective of stone type. Urine pH plays a critical role in stone composition. Acidic urine promotes UA and cystine stones, whereas alkaline urine promotes calcium phosphate and struvite stones. A simple test performed during an outpatient visit is all it takes to measure urine pH. However, urinary pH fluctuates over a 24-hour period, typically increasing after meals, and dropping <5.5 in periods of fasting. Therefore, urine normally is alkaline during the day and slightly acidic in the early morning and late at night.
Patients who form UA stones most commonly have persistently low urine pH, <5.5, along with a loss of the normal post-prandial alkaline tide. To measure alkaline tide, labs should check the pH of fresh urine periodically over a 24-hour period. If the patient's urine pH is 4.5–6, alkali therapy is indicated. This type of assessment also is used to monitor therapy.
Urine culture is another important element of assessing patients. The presence of infection can lead to struvite stones and low urine citrate.
The cornerstone of kidney stone biochemical evaluations is a 24-hour urine analysis. The results provide important prognostic information, guide preventive recommendations, and aide in monitoring therapy. Generally speaking, labs should obtain two 24-hour urine collections for comparison, as mineral excretion varies from day-to-day.
A patient's urine output is also an important indicator. Low urine volume increases the risk of stone formation. Between 12–25% of first-time stone formers have low urine excretion volume, defined as <1 L/24 hours.
|
Table 2
Biochemical Investigations of Patients with Kidney Stone Risk Factors
|
| Investigation |
Risk Factor for Stone Formation |
| Blood |
| Calcium |
Hypercalcemia (primary hyperparathyroidism, vitamin D toxicity, sarcoidosis) |
| Urate |
Hyperuricemia (gout) |
Potassium
Bicarbonate
Chloride |
Hyperchloremia with hypokalemia and low bicarbonate (distal renal tubular acidosis) |
| Phosphate |
Hypophosphatemia (renal phosphate leak) |
| Creatinine |
Chronic kidney disease |
|
24-hour Urine
|
| Urine Volume |
Low urine volume promotes urine supersaturation |
| Calcium |
Hypercalciuria |
| Phosphate |
Phosphaturia |
| Sodium |
High urinary sodium |
| Oxalate |
Hyperoxaluria |
| Citrate |
Hypocitraturia |
| Uric Acid |
Hyperuricosuria |
| Magnesium |
Hypermagnesiuria |
| Cystine |
High urinary cystine |
Other Biochemical Investigations
Traditionally, the dRTA work-up has included an ammonium chloride load test, which, though considered the gold standard test, frequently causes nausea and vomiting. Alternatively, labs can use the frusemide acidification test that has excellent sensitivity and specificity as a screening test, at 100% and 82%, respectively. Frusemide loads the renal proximal tubule with sodium, which is then reabsorbed in exchange for H+, resulting in urine acidification in normal patients.
A fasting urine pH >5.5 with no evidence of urinary tract infection is suggestive of dRTA. These results should be confirmed with 40 mg of frusemide administered orally to the patient and urine samples collected every 30 minutes for 3 hours. Urine of normal patients will be acidic, pH <5.5, but in those with dRTA, it will be >5.5.
Another useful test is maximum tubular reabsorption of phosphate, which is defined as the ratio of the phosphate reabsorption to the glomerular filtration rate (TmP/GFR). This calculation is useful for assessing renal phosphate reabsorption in patients with associated phosphaturia not caused by hyperparathyroidism. Patients fast overnight and both urine and serum samples are collected to measure phosphate and creatinine levels. The normal TmP/GFR ratio for adults is 0.8–1.35 mmol/L.
Analysis of Stone Composition
Analysis of the stones retrieved from patients represents a biochemical biopsy of the urinary environment at the time of crystal deposition and helps define risk factors or specific diseases leading to their formation. Stone composition may change, however, due to treatment. For example, patients with cystine or uric acid stones may form stones composed of calcium phosphate as a result of overly aggressive alkali therapy.
Numerous approaches are available to analyze kidney stones. Wet chemical analysis (WA) is the most widely employed technique. Although quantitative WA identifies the common stone components, it may miss rare and unidentified materials. Sophisticated techniques, such as X-ray diffraction crystallography, infrared spectroscopy, and scanning electron microscopy with energy dispersion, provide highly accurate stone analysis. Infrared spectroscopy also has the ability to generate accurate quantitative analysis.
Preventing Recurrence
Biochemical investigations of patients with kidney stones are important for discovering underlying risk factors for stone formation, as well as for directing appropriate treatment and monitoring it. While surgical treatments for kidney stones, such as ESWL and endoscopic laser stone fragmentation, attempt to remove the stone, these procedures do not tackle the underlying cause of stone formation or prevent recurrence.
In the urology community today, the general consensus is that patients with a high risk of stone recurrence should undergo extensive metabolic stone evaluation. Various studies have shown that such efforts not only reduce stone recurrence but also are cost-effective. In fact, many hospitals now have dedicated metabolic stone clinics.
Clearly, over the last few decades, much progress has been made in understanding the pathophysiology, diagnosis, and management of kidney stones. Both clinically and economically, metabolic stone evaluation plays a vital role in the treatment and prevention of kidney stones.
SUGGESTED READING
Castle SM, Cooperberg MR, Sadetsky N, et al. Adequacy of a single 24-hour urine collection for metabolic evaluation of recurrent nephrolithiasis. J Urol 2010;184:579–83.
Cicerello E, Merlo F, Gambaro G, et al. Effect of alkaline citrate therapy on clearance of residual renal stone fragments after extracorporeal shock wave lithotripsy in sterile calcium and infection nephrolithiasis patients. J Urol 1994;151:5–9.
Keevil BG, Thornton S. Quantification of urinary oxalate by liquid chromatography tandem mass spectrometry with online weak anion exchange chromatography. Clin Chem 2006;52:2296–99.
Keevil BG, Owen L, Thornton S, et al. Measurement of citrate in urine using liquid chromatography tandem mass spectrometry: Comparison with an enzymatic method. Ann Clin Biochem 2005;42:357–63.
Lifshitz DA, Shalhav AL, Lingeman JE, et al. Metabolic evaluation of stone disease patients: A practical approach. J Endourol 1999;13:669–78.
Reynolds TM, Burgess N, Matanhelias S, et al. The frusemide test: Simple screening test for renal acidification defect in urolithiasis. Br J Urol 1993;72:153–6.
Samuell CT, Kasidas GP. Biochemical investigations in renal stone formers. Ann Clin Biochem 1995;32:112–22.
Shekarriz B, Stoller ML. Uric acid nephrolithiasis: Current concepts and controversies. J Urol 2002;168:1307–14.
Stamatelou KK, Francis ME, Jones CA, et al. Time trends in reported prevalence of kidney stones in the United States: 1976-1994. Kidney Int 2003;63:1817–23.
Strohmaier WL. Economic aspects of evidence-based metaphylaxis. Urologe A 2006;45:1406–9.

Vinita Mishra, MBBS, MD, MPhil, FRCPath, is a consultant chemical pathologist at Royal Liverpool and Broadgreen University Hospital in Liverpool, U.K.
Email: [email protected]

Kee Wong, MBChB, MRCS, is a urology clinical research fellow at Royal Liverpool and Broadgreen University Hospital in Liverpool, U.K.
Email: [email protected]
Disclosure: The authors have nothing to disclose.