An effective laboratory stewardship roadmap includes a vision for a culture of laboratory stewardship in the organization. Stewardship initiatives often are driven from a system level, but most have their genesis within the laboratory and garner support in a bottom-up approach. Such strategies push laboratories to continually quantify the laboratory’s value within the health system.
In order to meet their objectives around appropriate test ordering, financial coverage, and improving patient care, laboratory stewardship programs should have four key elements, modeled mainly after antibiotic stewardship programs: (a) governance, (b) interventions, (c) data extraction and monitoring, and (d) review of data coupled with strategies and tactics for improvement (1). Laboratories often struggle with creating a strong governance structure that ensures sustainability for their stewardship program.
Great governance functions as an institution’s stewardship roadmap and includes a well-defined plan of action that defines problems and desired outcomes, aligns goals, plans specific interventions, and establishes ongoing process improvement and maintenance. Building a robust, sustainable, and effective program can be challenging, but with the right vision and a strong interdisciplinary stewardship committee, the impact can be sizeable.
Starting Strong: Establishing a Planning Committee
The planning committee offers direction about what the stewardship committee is trying to accomplish. This group’s goals include developing the mission statement, vision, scope, and objectives for the lab stewardship program; analyzing test utilization data to determine and prioritize opportunities for improvement; and identifying appropriate members for the lab stewardship committee.
Keep the planning committee small, usually 4−7 people, to effectively formulate goals and organize the main stewardship committee. The planning committee should include at least one clinician who frequently orders laboratory testing, a member from information technology (IT), a member from executive leadership, and a clinical laboratorian with an MD or PhD. Earning buy-in from all planning committee members is critical. This committee should meet 3−5 times.
Best Practices for the Laboratory Stewardship Committee
Organizations such as the Clinical and Laboratory Standards Institute (CLSI) and Seattle Children’s Patient-centered Laboratory Utilization Guidance Services (PLUGS) recommend multidisciplinary teams for utilization/stewardship efforts (1, 2). Laboratory representation is important, but a stewardship committee should be pathology supported, not led. It should include broad, high-ranking representation from medical and administrative leadership, and it is essential that the chief medical officer (CMO) and chief financial officer (CFO) participate or provide appropriate, visible, empowered designees. The most successful steering committees are at least cochaired by someone other than a pathologist, such as a clinician in a leadership position.
In a recent study of 47 survey respondents who rated the success of their stewardship programs, several who rated their program as “somewhat successful” or “very successful” highlighted the importance of multidisciplinary teams being a contributor to their program success (2).
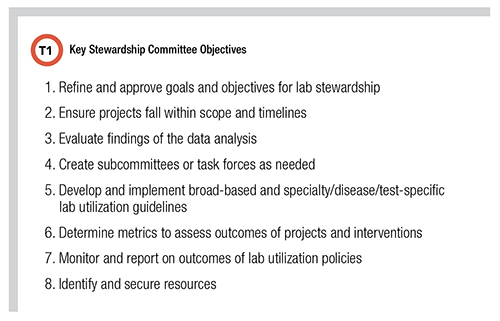
The stewardship committee should report to a higher-level committee, such as the medical executive committee (MEC) or utilization review committee. This allows the program to have greater visibility, tie efforts and activities to organizational strategic priorities, create accountability for participants, and improve access to resources (Table 1).
Dealing With Common Governance Problems
Improved governance can help solve some common problems that arise during the implementation of a laboratory stewardship program. These issues include poor communication of program purpose; lack of time/scheduling challenges; ineffective leadership; lack of support or resources; resistance from medical staff; and data/analytics procurement and analysis.
Analytics solutions can be a particular pain point. These include methods for data extraction, analysis of test data, and cost-savings projections. As they are critical to supporting the business case for stewardship, labs should consider their data needs early and often prior to implementing stewardship intervention (3).
The purpose of a test utilization data analysis is to improve patient care with cost-savings solutions that optimize lab utilization and minimize downstream impact, as well as demonstrate the value laboratory services bring to the health system. When laboratories are continually caught in strategies related to budget reductions, they can’t focus on larger opportunities in the value-based care model (4). A detailed review of test and provider utilization will assist with identifying stewardship opportunities; however, one of the most significant challenges when developing laboratory interventions to support value-based care is the need for analytics support.
Laboratory information systems (LIS) generally lack the ability to provide clinically meaningful analytics. Therefore, coordination outside of the laboratory is imperative to the success of stewardship initiatives. In particular, IT support is essential because identification of appropriate test utilization depends on access to data, evaluation of utilization depends on review of pre- and post-intervention data, and many stewardship interventions rely on IT support for implementation (4).
There are several strategies to consider for meeting these challenges. The most impactful is to assign a project manager to the stewardship committee. An effective project manager can have a tremendous impact on the success of coordinating program efforts and related activities.
Additionally, tying stewardship efforts to overall organizational strategic goals and priorities is a great way to engage at multiple levels of organizational leadership and garner support. Leveraging motivated hospitalists, residents, and fellows to drive stewardship committee tasks forward is a great way to keep momentum. Create ample opportunities for providers to bring issues to the laboratory. When they do, invite them to present to the stewardship committee.
Lastly, communicate frequently with executive and clinical leadership teams about the progress, outcomes, and opportunities related to your laboratory stewardship program.
How to Improve Collaboration With Providers
Participating in other provider-led, multidisciplinary committees such as pharmacy, quality, risk management, infection control, nursing, and administration allows the laboratory to better understand the varying needs of the organization and how clinical practice impacts laboratory utilization. If participating in a committee is not available, consider setting monthly or quarterly standing meetings to round with clinical service lines to address service-level needs.
Inviting specialty and subspecialty providers to participate as subject matter experts on the committees or subcommittees is another way to enhance collaboration and allow for their voice to be considered by a group of peers in decision-making. You might also consider partnering with a physician advisor or case-management team to improve metrics related to patient care.
Laboratorians have many opportunities to provide valuable clinical expertise related to laboratory testing, and these opportunities should be exploited to establish a collaborative committee focused on implementing evidence-based best practices, eliminating variation in care, increasing efficiency and efficacy of treatment, and eliminating unnecessary testing.
Tony Smith, BS(HCM), MLT(ASCP), is a senior healthcare consultant for Healthcare Advisory Services at ARUP Laboratories in Salt Lake City. +Email: [email protected]
References
- Dickerson JA, Fletcher AH, Procop G, et al. Transforming laboratory utilization review into laboratory stewardship: Guidelines by the PLUGS National Committee for Laboratory Stewardship. J Appl Lab Med 2017; doi: 10.1373/jalm.2017.023606.
- Dickerson J and Jackson B. Clinical Laboratory News. Improving quality while reducing costs: The art of laboratory stewardship. https://www.myadlm.org/cln/articles/2017/october/improving-quality-while-reducing-costs--the-art-of-laboratory-stewardship (Accessed December 2022).
- Swanson K. Today’s Clinical Lab. The hidden value in the clinical lab. https://www.clinicallab.com/trends/the-future-of-the-clinical-lab/the-hidden-value-in-the-clinical-lab-117 (Accessed December 2022).
- Kroner GM, Richman S, Fletcher A, et al. Current state of laboratory test utilization practices in the clinical laboratory. Acad Pathol 2022; doi.org/10.1016/j.acpath.2022.100039.