Penn State Hershey Medical Center, a leading tertiary care academic medical center in Hershey, Pennsylvania, has over 1 million outpatient visits annually, with our pathology and laboratory medicine department performing about 4 million tests per year. The department serves as a reference and consulting laboratory for Penn State Health system with 24-hour in-house coverage by physician-level anatomic and clinical pathologists, PhD-level clinical scientists, clinical fellows, pathology residents, and highly trained medical technologists and laboratory supervisors. The department has a fully operational automated testing laboratory for clinical chemistry, hematology, and coagulation analyses and also offers molecular diagnostics and mass spectrometry assays. In addition, we have price and/or service agreements with at least five vendors for sending out tests not performed in-house.
Deep Data Dive
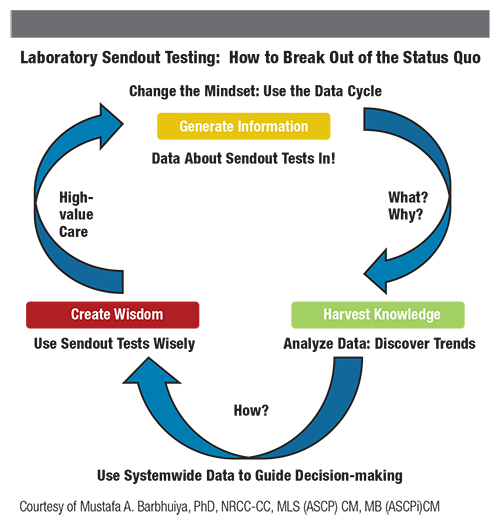
There had been limited systematic cost-benefit analysis of our sendout tests until we retrospectively reviewed sendouts over a 2-year time frame. We retrospectively considered tests to our two primary vendors in two year long time periods, then prospectively analyzed data for another year. Our goal was to identify why and which tests we were sending out and how they were positively and/or negatively impacting patient care, to determine the costs involved and which vendor was most cost-competitive, and to identify what else we could do to practice laboratory medicine more efficiently. I led the project and served on the project team along with our sendout test area medical technologist, laboratory manager, laboratory informatics team, and attending pathologists. Our data mining efforts helped us recognize a price discrepancy between our primary vendors and make an informed choice for our ongoing sendout needs.
Cost Differential Revealed
In our first retrospective review period (July 2016 to June 2017), we found that we sent out to two vendors 65,123 tests comprising 1,549 test types. Vendor A, a for-profit commercial laboratory, processed 984 test types and 43,853 total tests while Vendor B, a not-for-profit academic-based reference laboratory, handled 565 test types and 21,270 overall tests. The average cost of test per unit of test (independent of the type of test) was $54 for Vendor A and $32 for Vendor B, meaning Vendor A’s average cost per unit was 69% ($22) more than Vendor B’s. If we had sent out all tests in that period to Vendor B, we would have saved approximately $1 million.
Examples of the cost discrepancies include: Tissue Transglutaminase Ab, IgA (Vendor A, $24 versus Vendor B, $7); Hepatitis A Ab-Total (Vendor A, $10 versus Vendor B, $8); Pancreatic Elastase 1 (Vendor A, $175 versus Vendor B, $98); and Myositis Assessor Plus panel (Vendor A, $718 versus Vendor B, $395).
Based on these observations we established a sendout order preference for Vendor B. In the ensuing year (July 2017 to June 2018), we sent out to both Vendor A and Vendor B a total of 69,901 tests covering 1,292 test types. However, we sent out substantially more tests to Vendor B in comparison to Vendor A—59,774 orders of 820 different tests versus 10,127 orders of 472 different tests, respectively. The average cost per unit order for Vendor B was $34.34, while Vendor A’s was $111.88. Even though we substantially upped our testing volume with Vendor B, our annual cost increase per unit billed was negligible. In contrast, this cost increased more than twofold with Vendor A. Notably, both vendors handled tests across the range of costs per test. In that year compared to the previous year, we saw an overall reduction of 16% of sendout test types (1,549 tests to 1,292 tests).
In addition to shifting more volume to Vendor B, our analysis led us to bring some tests in-house. For example, we implemented a BCR-ABL-1 reverse transcription-polymerase chain reaction assay, along with free prostate specific antigen, hepatitis C virus antigens and antibody panels, and hepatitis C and A virus molecular assays. We are considering bringing inhouse other assays; our feasibility studies are ongoing.
This outcome is a continuous effort in our department to bring tests in-house as part of our mission to practice value-based laboratory medicine to improve turnaround times and patient care. Overall, through this project, we tried to achieve various goals of value-based healthcare delivery like strategic reduction in costs for patients and hospitals while providing improved healthcare, achieving higher efficiencies for laboratory medicine professionals as healthcare providers, and increasing patient satisfaction. Comparative studies such as ours will be the way forward in a value-based laboratory medicine practice.
Dr. Barbhuiya will discuss this topic during two roundtable talks (session numbers 42133 and 52233) at the 2020 AACC Annual Scientific Meeting on December 14.
Mustafa A. Barbhuiya, PhD, NRCC-CC, MLS (ASCP) CM, MB (ASCPi) CM, is clinical chemistry fellow in the Department of Pathology and Laboratory Medicine at Penn State University College of Medicine in Hershey, Pennsylvania. He is founder and director (pro-bono) of the global nonprofit organization Foundation for Advancement of Essential Diagnostics. +Email: [email protected]; [email protected]
Ronald E. Domen, MD, FACP, FCAP, is professor of pathology, medicine, and humanities at Penn State University College of Medicine/Hershey Medical Center in Hershey, Pennsylvania. +Email: [email protected]
The authors gratefully acknowledge the contributions of Donna Stutzman, MT, Thomas Stipe, MT, and Tony Douventzidis, MT, for their help in data collection. Mustafa Barbhuiya also acknowledges Yusheng Zhu, PhD, DABCC, FADLM, for mentorship and oversight, with special thanks to Michael H. Creer, MD, FASCP, FCAP.