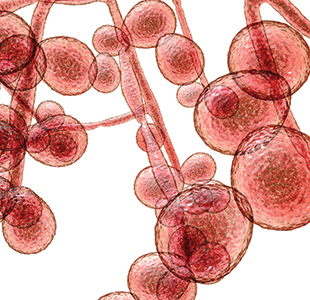
The COVID-19 pandemic has been top-story news throughout 2020, but another pathogen, Candida auris, has made headlines in recent years for its ability to cause outbreaks of severe illness in healthcare settings. Discovered in 2009, this fungus appears to have emerged nearly simultaneously on multiple continents. The U.S. Centers for Disease Control and Prevention (CDC) reports that as of June 30, 2020, 1,208 clinical cases have been confirmed in the United States. Interestingly, some states, such as Illinois, New York, and New Jersey, have experienced hundreds of cases, while others have seen none. The rapid global expansion of this mysterious fungus has forced clinical labs to swiftly adopt the specialized laboratory methods needed to identify it and curb further transmission.
“With a pathogen like C. auris, which can colonize the skin and spread easily within healthcare facilities, rapid detection from the laboratory is key,” said Elizabeth Berkow, PhD, laboratory director for the Mycotic Diseases Branch at CDC. Indeed, even as SARS-CoV-2 (the cause of COVID-19 illness) makes unprecedented demands on clinical labs’ time and resources, prompt and accurate identification of C. auris remains key to preventing outbreaks.
MALDI-TOF versus PCR
Traditional phenotypic methods for identifying yeast can mislabel C. auris as a number of other organisms, including other pathogenic Candida species. In light of this, clinical labs have two main approaches for identifying C. auris: matrix-assisted laser desorption/ionization time-of-flight (MALDI-TOF) mass spectrometry–or polymerase chain reaction (PCR)–based methods. “Both are good ways to identify C. auris,” said Kenneth Van Horn, PhD, technical director of microbiology at the Southern California Permanente Medical Group in Chino Hills.
Currently, however, “clinical laboratory capacity for C. auris testing in the United States exists on a wide spectrum,” noted Berkow. Many smaller clinical labs are not set up for either MALDI-TOF or PCR-based methods of identifying C. auris. According to proficiency testing data from the College of American Pathologists, “about half of clinical labs use MALDI-TOF to identify yeasts, such as C. auris, recovered in clinical specimens, about half use phenotypic methods, and at this time few laboratories use PCR-based methods,” said Carey-Ann Burnham, PhD, professor of pathology and immunology, molecular microbiology, pediatrics, and medicine at Washington University School of Medicine in St. Louis..
Labs that still rely on traditional phenotypic methods of identifying yeast should be aware of the C. auris mimics and be on high alert when one is detected, Burnham cautioned. “If you see one of those mimics, if confirmatory methods are not available in your own laboratory, it is really important to reach out to your public health reference laboratory,” she said. “Develop a relationship well in advance, so that if something happens, you have that relationship and know what to do.”
Any U.S. clinical lab in need of support should reach out to CDC’s Antibiotic Resistance Laboratory Network, stressed Berkow. This network of seven laboratories screens patient samples for C. auris according to CDC protocols.
Most clinical labs favor MALDI-TOF-based methods to identify C. auris for several reasons. Many labs already routinely use MALDI-TOF systems to identify other microorganisms, according to Van Horn, so they are convenient. Also, the consumables required for this type of testing are inexpensive, usually less than $1 per isolate tested.
These advantages aside, MALDI-TOF testing requires that an isolate be grown from culture, which takes approximately 7 days, though the test itself can provide results within minutes. In addition, not all MALDI-TOF reference libraries enable C. auris detection. “The number one thing you need to be aware of is whether C. auris is even in your MALDI-TOF library or database,” said Burnham. On its website, CDC specifies which reference libraries are suitable for identifying C. auris. Users who do not have access to an appropriate device manufacturer’s library can use CDC’s MicrobeNet database, available for free online.
PCR-based testing has a leg up on MALDI-TOF in that it can be used directly on specimens, avoiding the need for cultures. This translates into faster turnaround times, as well as potentially greater sensitivity, said Susan Poutanen, MD, MPH, a professor of laboratory medicine at the University of Toronto. However, if a specimen yields a positive result, “labs would still need to culture the sample to be able to obtain the organism’s full susceptibility profile,” she cautioned.
PCR-based testing would receive higher marks but for the resources it requires. Today, public health or reference labs are the primary users of this type of analysis. “Many clinical laboratories do not have the equipment or capability to perform PCR testing,” said Van Horn, observing that PCR-based C. auris identification might be quite expensive and to the best of his knowledge no commercial vendors currently offer this type of testing.
Labs that perform PCR-based identification have two overall options. In general, “larger laboratories and reference centers perform broad-range fungal PCR with DNA sequence-based identification,” according to Gary Procop, MD, MS, medical director of the molecular microbiology, mycology, parasitology, and virology laboratories at Cleveland Clinic. However, C. auris-specific PCR protocols are also available, including from CDC.
A New Option
Recently, a new testing option has become available to clinical labs that test blood specimens for C. auris. In late 2018, the Food and Drug Administration (FDA) approved the GenMark ePlex Blood Culture Identification Fungal Pathogen panel. If a blood culture is found to contain yeast using a Gram stain, the specimen can then be processed using the panel, which employs microarray hybridization to detect microorganism-specific signature sequences, including those of C. auris, explained Procop.
Susceptibility Testing
According to the Infectious Diseases Society of America, all clinically relevant Candida isolates should undergo antifungal susceptibility testing. C. auris is often multidrug resistant, but levels of antifungal resistance vary widely between isolates. Concerningly, several have demonstrated resistance to all three classes of antifungals.
Despite C. auris’s real and present danger for resistance, antifungal susceptibility testing doesn’t always happen, said Burnham, especially by smaller labs that are not equipped to carry out such testing for fungal pathogens. Susceptibility testing for some antifungal agents is challenging due to a lack of breakpoints for those drugs, which limits approval for these tests by FDA. Consequently, labs might be limited to testing isolates’ susceptibility to a small number of antifungal agents—or none at all.
However, CDC offers tentative breakpoints to assist labs in performing C. auris susceptibility testing, said Berkow.
Action Steps
Whenever a facility has a suspected or confirmed case of C. auris, rapid action is the name of the game. Nursing and infection prevention teams need to be notified swiftly, so that they in turn can immediately implement appropriate infection prevention protocols, stressed Teri Caughlin, RN, MHA, regional director of infection prevention for Southern California Kaiser Permanente in Pasadena. These protocols typically include contact precautions, personal protective equipment (PPE), and Environmental Protection Agency-approved surface cleaning products effective against C. auris. The latter matters because even products with fungicidal claims might not kill C. auris.
Establishing point prevalence and conducting contact tracing and admission screening also are essential elements for controlling the spread of C. auris, added Sudha Chaturvedi, PhD, director of the Mycology Laboratory at the New York State Department of Health’s Wadsworth Center in Albany. All of these strategies depend on the availability of swift and accurate testing, she stressed.
Although some hospitals in high prevalence areas might routinely test all patients for C. auris colonization, others might not do so until they have a positive case. This type of epidemiologic search is critical, said Procop: “The clinical isolate may be the tip of the proverbial iceberg.”
Two Potent Microbes
Some evidence suggests that the COVID-19 pandemic could exacerbate C. auris transmission in healthcare facilities. PPE shortages, or changes in infection control practices spurred by concerns about future shortages, could allow the fungus to spread. “This has been observed in long-term care facilities, as well as acute care hospitals, which typically had less C. auris transmission prior to the COVID-19 pandemic,” said Meghan Lyman, MD, epidemiologist at CDC.
Facilities also can’t take for granted that the same procedures that curb the spread of SARS-CoV-2 will work for C. auris. For example, “disinfectants recommended for use against COVID-19 in the United States are either ineffective against C. auris or have not yet been tested for effectiveness,” warned Berkow.
However, improved hand hygiene due to the COVID-19 pandemic has benefited patients by reducing the transmission of non-COVID pathogens, said Caughlin. And the COVID-19 pandemic might not have compromised the ability to detect C. auris in facilities like Van Horn’s with dedicated mycology labs, he suggested.
“We will have a clearer picture of what, if any, impact the COVID-19 pandemic has had on C. auris control later in the year,” added Chaturvedi.
The Future of C. auris Testing
Because C. auris is a relatively novel pathogen, the testing landscape is still evolving. Developing affordable, widespread commercial PCR testing that rapidly screens specimens will be important, said Van Horn.
“Molecular testing is the way to go for rapid detection and prevention,” agreed Chaturvedi, whose laboratory has developed a rapid, high-throughput real-time PCR assay for detecting C. auris.
Procop expects additional commercial vendors to join GenMark in adding C. auris to their diagnostic panels, and Van Horn hopes to see low-tech approaches accessible to all labs developed as well. One possibility, he said, might be an inexpensive culture-based method of screening, such as a chromogenic agar plate.
For its part, CDC is focusing on testing platforms that will increase throughput and reduce hands-on time for technologists, said Berkow. With these types of advances, healthcare facilities will be better able to identify and mitigate C. auris.
Kristin Harper is a freelance writer in Seattle, Washington. +Email: [email protected]