Diagnosticians are working alongside clinicians in supporting optimal care for patients with COVID-19. Routine laboratory markers provide key insights into this illness, contributing to patient admission protocols, guiding treatment, and assessing patients’ risk of severe disease. Here at Kokilaben Dhirubhai Ambani Hospital & Medical Research Institute in Mumbai, India, we have undertaken a study evaluating routine laboratory biomarkers in COVID-19 patients admitted with positive SARS-CoV-2 test results by real-time reverse transcriptase polymerase chain reaction (rRT-PCR).
Our study involved 528 subjects—370 males (70%) and 158 females (30%)—with a median age of 61 years, ranging from 12 to 93. We performed serial measurements of at least 22 routine laboratory biomarkers, such as aspartate aminotransferase (AST), alanine aminotransferase (ALT), C-reactive protein (CRP), procalcitonin (PCT), cardiac troponin measured with a high-sensitivity assay (hs-cTn I or T), and lactate dehydrogenase (LDH).
In COVID-19 cases versus controls, we found significant increases in mean values of AST, ALT, total bilirubin, creatinine, CRP, PCT, LDH, interleukin-6 (IL-6), ferritin, lactate, hs-cTn I, and N-terminal pro B-type natriuretic peptide and decreases in mean values of albumin, saturated oxygen, and neutrophil lymphocyte ratio. We applied a receiver operating characteristic (ROC) curve to discriminate the case population more precisely than the control population.
Because severe COVID-19 has been linked to raging cytokine storm syndrome, we also performed serial measurements of analytes that might offer insights into this condition, including not only CRP, D-dimer, and ferritin but also cytokine tests, particularly IL-6.
Severe Illness in Two Cases
Not every country has sex-specific data, but a clear trend has emerged in some places, including at our institution where we have seen not only a higher percentage of male patients but also a higher percentage of men experiencing more severe illness. The disease distribution also varies according to ethnicity. To explain the role of routine laboratory parameters in COVID-19 disease monitoring, we present below two cases involving an elderly female and an elderly male patient. Both cases also show that cytokine storm can affect both men and women.
Case 1: A Woman With Hypertension
An elderly female with a history of hypertension presented to the hospital complaining of breathlessness and fever for 2–3 days, along with generalized weakness. She did not have a history of recent travel or SARS-CoV-2 contact but was confirmed for COVID-19 through rRT-PCR testing. Her ECG showed changes in ST waves and T waves, in anterior and lateral leads. High-resolution CT scanning detected bilateral subpleural ground glass opacities, associated with small consolidations and crazy paving mainly in the right lobe, typical of viral infection.
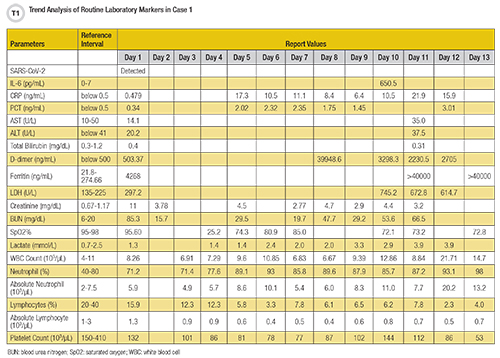
This patient’s laboratory findings supported the diagnosis of severe COVID-19 illness with elevated levels of ferritin (389.7 ng/mL), IL-6 (9.83 pg/mL), D-dimer (1,555.94 ng/mL), creatinine (1.34 mg/dL), hs-cTn I (130.6 ng/L), and CRP (3.33 mg/dL) (Table 1).
Case 2: A Man With Diabetes
An elderly male with diabetes, hypertension, and chronic kidney disease on maintenance hemodialysis presented to the hospital complaining of very high-grade fever for 3 days along with breathing difficulty and generalized weakness. The patient had no recent travel or SARS-CoV-2 contact history. He tested positive for SARS-CoV-2 by rRT-PCR from a nasopharyngeal swab, and his chest X-ray showed bilateral lung infiltrates.
This patient’s routine laboratory findings supported the diagnosis of severe COVID-19 illness with elevated levels of IL-6 (650.5 pg/mL), CRP (17.3 ng/mL), PCT (2.02 ng/mL), hs-cTn I (45.9 pg/mL), D-dimer (3,298.31 ng/mL), ferritin (>40,000 ng/mL), LDH (745.2 U/L), creatinine (4.5 mg/dL), blood urea nitrogen (29.5 mg/dL), neutrophil count (85.7%), absolute neutrophil count (11 X 103/µL), lactate (3.3 mmol/L) and decreased levels of albumin (3.62 g/dL), total protein (6.3 g/dL), saturated oxygen (85.2%), lymphocyte count (6.2%), absolute lymphocyte count (0.8 X 103/µL), and platelet count (132 X 103/µL).
An Insight Into IL-6
In individual cases and in our study overall, we have found IL-6 measurements to be particularly useful in discerning worsening COVID-19. For example, in a third case involving a severely ill patient, a trend analysis of IL-6 found this analyte reaching a trough of 524 pg/mL 2 days after admission from a baseline of 2,766 pg/mL, then rebounding over the next 2 days to 1,056 pg/mL, while other markers of inflammation such as PCT, CRP, and D-dimer steadily declined. Ferritin joined IL-6 in an unfavorable trajectory, rising from a baseline of 4,097 ng/mL to 5,828 ng/mL 3 days later.
An ROC analysis to discriminate between COVID-19 cases admitted to intensive care versus healthy subjects found the ROC for IL-6 to be 1.0 with 95% confidence interval and a P-value <0.0001. In box plots of the IL-6 data from the case group, the first quartile (25th percentile) and third quartile (75th percentile) were 33.56 pg/mL and 295.15 pg/mL, respectively, with an interquartile range of 261.58 pg/mL, a median of 76.86 pg/mL, and whiskers to 7.24 pg/mL and 679.1 pg/mL. This illustrates the important role cytokines play in inflammatory and immunological response regulation.
The COVID-19 pandemic has notably underscored the essential role that we as diagnosticians play not only in identifying SARS-CoV-2 infections but also in supporting clinicians working strenuously to effectively manage patients with COVID-19 who exhibit a considerable spectrum of illness.
Barnali Das, MD, DNB, PGDHHM, is a consultant in laboratory medicine at Kokilaben Dhirubhai Ambani Hospital & Medical Research Institute in Mumbai, India. She also is an executive member of the scientific division of the International Federation of Clinical Chemistry and Laboratory Medicine and chair of AACC’s India section. +Email: [email protected]
The author gratefully acknowledges Seema Y. Bhatia, Poonam Mandavkar Pal, Rashmi Patil, Vishakha Tawde, and Poornima Shetty and thanks all laboratory medicine department team members at Kokilaben Dhirubhai Ambani Hospital & Medical Research Institute.