With clinical laboratories facing constant reimbursement pressures—which seem likely to be exacerbated when a new market-based Medicare payment system for lab tests takes effect in 2018—finding ways to improve efficiency and reduce costs in the core lab is not only desirable, but necessary. To deal with these pressures, more labs now are reconsidering automation—and with good reason. Labs can reduce staffing by up to 30% through automation, according to Robin Felder, PhD, associate director of laboratory medicine at the University of Virginia in Charlottesville and a laboratory automation consultant.
At a time when the laboratory labor force is shrinking, the ability to do more with fewer workers is critical for survival. Felder reports that one hospital laboratory he worked with on an automation solution was able to reduce staffing by at least 50%, primarily through attrition. Automation clearly helps labs improve efficiencies and reduce costs, but the level of automation needed depends largely on each lab’s size, test volume, and budget. A basic automation system, which includes a feeder and an automated centrifuge, could cost at least $300,000, Felder noted, with a return on investment of 3 to 5 years. Since the life expectancy of automation equipment is about 10 years, labs investing in a basic system would achieve savings in the second 5 years.
But while the benefits of lab automation are clear, a significant percentage of clinical labs still have not implemented any automation, according to experts. This means there still are many across the country that have yet to achieve the efficiencies and cost savings that automation brings.
What Do I Really Need?
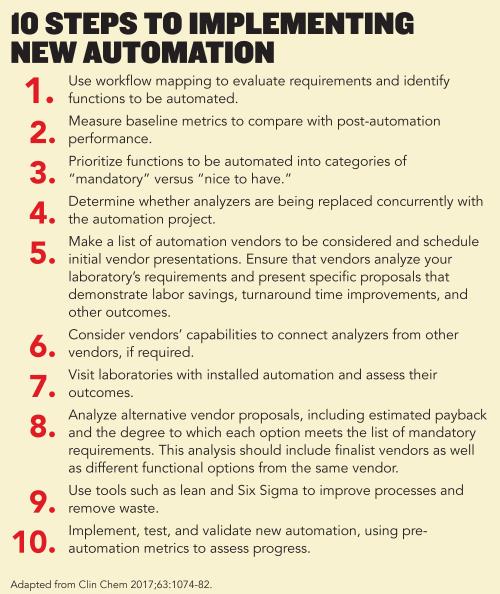
Before considering new automation or upgrading existing systems, laboratories should begin by closely evaluating their requirements, advised Charles Hawker, PhD, MBA, scientific director of automation and special projects at ARUP Laboratories in Salt Lake City. Labs should begin by mapping the current laboratory workflow from specimen receipt through reporting of results. This helps spot steps in the process that waste labor, create bottlenecks, or are prone to error (See box, p. 28).
If a lab determines that 80% of its daily workload is ripe for automation, it usually justifies the investment based on labor savings and improved turnaround time and quality, Hawker said. He also recommends that laboratories rely on lean and Six Sigma to ensure that automated solutions actually improve operations. “No one should just go buy automation and stick it on a poor process,” he said.
In addition to reducing errors, lean and Six Sigma also help improve efficiency. In the 12 years after ARUP Laboratories performed a lean analysis and automated in 1998, it saved 130 full-time equivalent positions, reduced turnaround times by 30% and decreased lost specimens from 6.5 per million to less than 0.1 per million, all while growing volumes by thirtyfold. “The efficiency improvement we’ve achieved over the years is mind-boggling,” Hawker said.
Once a lab has evaluated and streamlined processes, it’s time to decide what type of automation is needed. Depending on a lab’s size and budget, task-targeted automation (TTA), such as automating labeling or transport of specimens, may be a good choice. The other option is total laboratory automation (TLA) systems that use conveyors to link specimen processing functions to analyzers and often include post-analytical features.
Tasks that are repetitive and monotonous—and thus prone to human error—lend themselves to task automation. If a lab’s budget allows and specimen volume supports it, TLA may be the way to go. When TLA systems first became available in 1995, volumes of 15,000 to 25,000 specimens per day were required to justify an investment in automation, but those threshold volumes now have dropped to as low as 1,000 per day, Hawker noted. Task-targeted automation for specimen processing or other tasks can be justified on as few as 500 specimens per day (Clin Chem 2017;63:1074-82).
Exploring Task-Targeted Automation
With an ability to customize a product to fit a lab’s workflow and budget, vendors now offer a growing menu of TTA options. “Significant improvements in efficiency, quality, and turnaround time can be achieved by implementing a TTA system that either performs a single task or combines several tasks into a multi-function workstation,” Hawker said. TTA examples include automated centrifuges, decappers, recappers, aliquotters, and sorters, which can be used for both pre-analytical and post-analytical sorting for archival storage.
TTA almost always delivers a return on investment, Felder added, noting that it is most useful for error-prone repetitive and labor-intensive jobs. The cost of targeted equipment is also much less than a full automation system, he said, noting that an automated centrifuge could be purchased for less than $100,000.
In addition to single task systems, many vendors now offer multi-function TTA systems that automate several of the manual steps in a typical specimen processing function, such as receiving specimens, inspecting them for appropriateness, accessioning specimens into the laboratory information system, affixing a bar code label, and sorting urgent specimens from routine specimens. These functions might be a good choice for labs with daily workloads of 500 to 1,500 specimens or that use analyzers from different vendors, says Hawker.
Total Laboratory Automation
TLA systems use conveyor belts to connect pre-analytical specimen processing and other functions directly to an analyzer. Such systems may also include functions such as post-analytical storage or sorting of specimens or aliquots to be transported to low-volume testing areas—or to be sent to reference laboratories.
While TLA systems perform more functions than TTA systems, laboratories should balance the additional cost of TLA against the expected benefits, Hawker emphasized. “Some labs with a daily workload as low as 600 to 800 specimens have justified TLA systems because of a shortage of technical help,” he said. “But typically these systems are designed for laboratories with workloads of 1,000 to more than 25,000 specimens per day.”
Automation Trends
One of the challenges in automation has been developing systems that deal with different tube shapes and sizes, said Jonathan Genzen, MD, PhD, medical director of the automated core laboratory at ARUP Laboratories. Increasingly, vendors are working to engineer equipment that handles pediatric tubes and other tubes of unusual sizes.
Automated refrigerated storage and retrieval systems that enable laboratories to retain up to 1 week’s worth of specimens are also becoming more popular. Designed to hold 3,000 to 30,000 specimens, these systems can also feed biorepositories, giving researchers access to specimens.
Vendors also are making advances in mass spectrometry (MS) workflow automation, with MS instruments coupled to automated front-end technology. Developments in this area are likely to intensify in the coming years.
Machine vision technology—widely used in manufacturing—is the latest laboratory automation trend. This technology replaces human inspection, speeding production and reducing errors. In laboratories, machine vision sensors check tube heights, diameters, and stopper colors, examine spun tubes for the volume of serum, and determine the presence of interferences such as hemolysis, according to Hawker.
Felder is equally bullish on this emerging application. “I think specimen inspectors are the wave of the future,” he said. “This technology is already being used with a great deal of success in other sectors.”
Given the economic and staffing pressures, almost all laboratories are likely to adopt some form of automation as a way to increase efficiency and bring down costs. Whether your laboratory pursues TTA or TLA, chances are that some type of lab automation is in your future.
Kimberly Scott is a freelance writer who lives in Lewes, Delaware.+Email: [email protected]