Jaime Noguez, PhD, of the CLN Patient Safety Focus editorial board conducted this interview.
Physicians have always strived to provide individualized and safe care for their patients. But today’s healthcare environment increasingly makes it difficult for them to do so at the level necessary to prevent errors and adverse events. Clinical laboratories are in a unique position to help reduce this risk and use the power of technology to streamline care, catch and correct errors, enable a more rapid response to adverse events, and assist with clinical decisions.
However, many laboratorians are not sure where to start. In this interview, Eugenio Zabaleta, PhD, provides practical examples of how labs can use technology to enhance the value of laboratory results and improve patient care. Zabaleta is a clinical chemist at OhioHealth Mansfield and Shelby Hospitals.
How have you used information technology (IT) to improve patient safety?
Leadership at OhioHealth Mansfield and Shelby Laboratories understand that our laboratory has to play a more decisive role by providing clinical decision support (CDS) for laboratory orders and results. This not only contributes to patient safety but also makes the lab a critical part of the healthcare team.
In 2009 our laboratories implemented an automated critical value notification system—for example, identifying clinically significant changes in cardiac troponin results. When the software identifies the first increase of cardiac troponin, it sends an alert message to the laboratory information system. The performing lab professional then calls the patient’s nurse, who informs the attending physician. The software also sends the results to the physician through the electronic medical record (EMR) under the “Alert” section (1).
We also use CDS to identify patients with heart failure who could benefit from the OhioHealth Mansfield and Shelby Hospitals’ Heart Success program, developed in response to Medicare’s Hospital Readmissions Reduction Program. The software calculates a patient’s risk of re-admission and sends the results via email to our Heart Success personnel, along with patient demographic information, risk calculation, and other laboratory data (2).
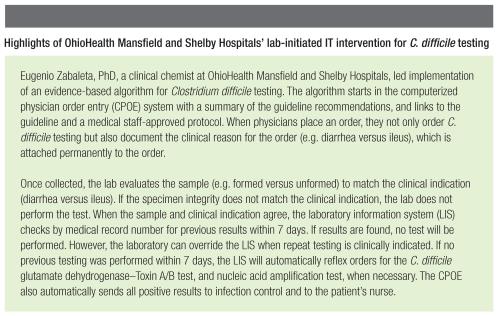
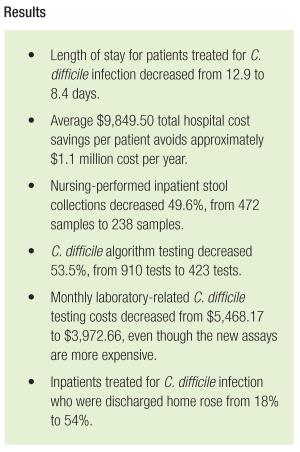
More recently, we implemented automated testing algorithms and evidence-based order sets for the health system’s computerized physician order entry (CPOE) software. In one of our most successful lab-initiated IT interventions, we created an algorithm for Clostridium difficile testing based on Infectious Diseases Society of America guidelines that improved care and reduced costs (3).
What challenges have you encountered working on these projects, and how did you overcome them?
The health system created my position in 2005 to improve the interactions between clinicians and the lab. As a liaison, the first barrier I faced was making physicians, nurses, and laboratorians comfortable with my role and the tools available to me.
At first I faced a lot of skepticism from physicians. They were not sure that the lab could help them at the bedside. My initial approach was to offer my laboratory medicine expertise to solve problems or adopt new regulatory challenges such as Centers for Medicare and Medicaid Services (CMS) core measures. I used peer-reviewed papers, copies of presentations, and magazine articles to show them how others were solving problems and how I could adapt these solutions for our hospital.
Once I overcame their skepticism I worked to gain their trust and respect by making every process improvement, quality project, or safety project a formal and structured process that applied the scientific method. Using the scientific method to implement improvements created a solid framework that enabled us to learn from our mistakes in an objective and structured way. I also emphasized the need for frequent, real-time communication among team members.
Making sustainable changes is very challenging when it involves interdepartmental collaboration. Every member of the team must have a voice and feel empowered to contribute without fear of criticism or that others will minimize their needs and concerns. For every project, I aimed to establish a strong lab-physician team based on three pillars: respect, equality, and understanding of each other’s strengths, weaknesses, workflow, and regulations. This teamwork structure helped us analyze processes as a whole—not just the individual responsibilities of each specialty.
What advice do you have for laboratorians trying to replicate your success?
The number 1 misconception about these interventions is that they are solely IT projects. Although IT is very important, it is just a tool to enhance the practice of medicine and increase patient safety. The human element cannot be overlooked! I believe strongly that communication among all the project’s stakeholders is the key to making these interventions effective and efficient. When implementing projects like this, you need to concentrate first on the medical evidence, physicians’ expertise and needs, and on the patient safety and quality improvement elements—only after those considerations does IT make its entrance.

Moreover, you have to show physicians that you are there to help them and their patients because you have unique expertise in laboratory medicine. It would help to find lab champions who are clinicians and share your vision. I am fortunate to have the support of our vice presidents of medical affairs, medical staff, laboratory services, and nursing.
I started forging these relationships by introducing myself via email. Then I scanned for regulatory changes, new CMS core measures, quality problems, and physicians’ dissatisfiers. Once I identified an opportunity, I developed a solution and presented it to these leaders as a formal proposal. I tried to follow up with a personal encounter, even informal hallway chats, so they could associate my name with my face. The leaders gave me a chance to do a pilot, then another, and another. Soon, clinicians and administrators brought their problems to me and invited me to participate in their committees.
I advise against getting caught up in an all-or-nothing approach to projects. Often, inspiring articles that describe how other organizations solve a common problem involve big teaching institutions with many resources. Not being in one of those institutions, I have a very different set of resources. But instead of giving up, my technique, which I call “The Frankensteinian Approach,” has been to adapt components of big institution solutions. This is not always easy, but it has worked well for me so far.
Jaime Noguez, PhD, DABCC, is the assistant director of clinical chemistry at University Hospitals Cleveland Medical Center and an assistant professor of pathology at Case Western Reserve University in Cleveland. +Email: [email protected]
References
1. Zabaleta E, Burgess J, Eaton G, et. al. Impacting patient care through laboratory decision support-
identification and alert of the patient’s first troponin-I increase. J Pathol Inform 2012;3:S50–S51.
2. Zabaleta E, Burgess J, Truax K, et. al. How can laboratories help their hospital decrease readmission rates for heart failure patients? J Pathol Inform 2012;3:S4.
3. Cohen S, Gerding D, Johnson S, et. al. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the Society for Healthcare Epidemiology of America (SHEA) and the Infectious Diseases Society of America (IDSA). Infect Control Hosp Epidemiol 2010;31:431–55.
CLN's Patient Safety Focus is sponsored by ARUP Laboratories
