As laboratory leaders, we are responsible for placing our staff in regular contact with patients. Laboratory staff interface with patients in a variety of ways: performing phlebotomy and heel sticks; performing special procedures on patients, such as sweat tests for cystic fibrosis; providing laboratory supplies to patients to bring home (such as urine cups, sputum cups, 24-hour stool or urine collection receptacles, and guaiac cards); demonstrating to parents or guardians how to place a urine bag on an infant for urine collection; and performing point-of-care (POC) testing with equipment at the patient’s bedside.
Even when no contact with patients occurs, the staff is at risk for occupational exposures from contact with patient specimens, including blood, body fluids, aerosol, and tissue. As for patients, approximately 1 in 25, or well over 700,000 a year in the U.S., contract hospital-acquired infections, according to the Centers for Disease Control and Prevention (CDC).
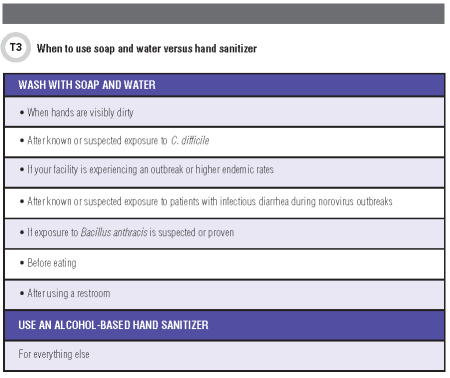
One of the best evidence-based ways to prevent these often serious and intractable infections is hand hygiene. I am often asked about what is required for hand hygiene—for example, when talking about POC settings. The most recent evidence-based guidance from CDC requires hand hygiene using an alcohol rub and in some cases hand washing with running water and soap (1).
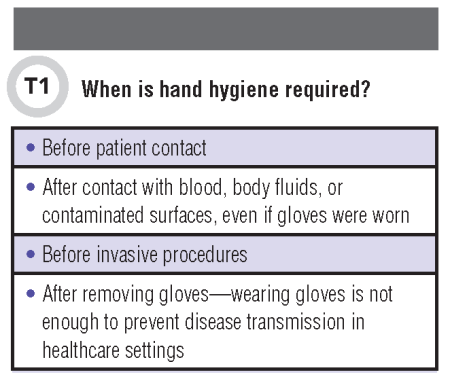
Broadly, there are four cardinal lessons from the most recent published literature on this topic. One of the first lessons from the evidence base is that hand washing is required more frequently than is commonly appreciated (Table 1).
The second lesson from current literature is that alcohol-based sanitizers—which have become routine instruments of hand hygiene in healthcare facilities—have significant limitations (Table 2).
Several reports describe the ingestion of hand sanitizers as a surrogate for potable alcohol by patients with a history of mental illness or substance abuse. Life-threatening intentional ingestion of an ethanol-based hand sanitizer is described in published case reports (2, 3). Reported hand sanitizer exposures among children numbered approximately 85,000 in 2011–2015, according to U.S. poison control centers (4). Analysis of reports to the American Association of Poison Control Centers National Poison Data System for exposures to ethanol-containing hand sanitizers reveal a rising incidence of purposeful ingestion of ethanol-containing hand sanitizers (5).
The third lesson is learning how hand washing is correctly performed.
Effective Handwashing
With an alcohol-based hand rub
1. Follow directions on the bottle for how much product to use.
2. First rub hands together, and then rub product all over the top of both hands, in between fingers, over the area around, and under the fingernails.
3. Continue rubbing until hands are dry. If adequate rub was used, it should take at least 15 seconds of rubbing before your hands feel dry, or the time it takes to sing the “Happy Birthday” song twice.
4. You should not rinse your hands with water or dry them with a towel.
With soap and water
1. Wet hands with warm water. Use liquid soap if possible. Apply a nickel- or quarter-sized amount of soap to your hands.
2. Rub hands together until soap forms a lather; then rub all over the top of hands, in between fingers and over the area around, and under the fingernails.
3. Continue rubbing hands for 15 seconds, or the time it takes to sing the “Happy Birthday” song twice.
4. Rinse hands well under running water.
5. Dry your hands using a paper towel if possible. Then use the paper towel to turn off the faucet, and to open the door if needed.
The fourth lesson is that hand washing is not just for healthcare providers. Patients and visitors are part of the hospital-acquired infection fighting team (Table 4).
Where do we go from here?
For many, the requirement for hand-washing with soap and running water and the frequency of doing so still represents change. Simple directives to staff and visitors alike can be surprisingly difficult to implement. Covert observation can best reveal quality gaps between procedures and practice, knowledge and behaviors (1). Measurement is recommended to insure progress is made and that interventions are effective.
References
1. CDC. Hand hygiene in health care settings. Show me the science. http://www.cdc.gov/handhygiene/science/index.html (Accessed August 15, 2016).
2. Miller M, Borys D, Morgan D. Alcohol-based hand sanitizers and unintended pediatric exposures: A retrospective review. Clin Pediatr 2009;48:429–31.
3. Rayar P, Ratnapalan S. Pediatric ingestions of household products containing ethanol: A review. Clin Pediatr 2013;52:203–9.
4. Georgia Poison Center. www.georgiapoisoncenter.org/hand-sanitizer/ (Accessed August 15, 2016).
5. Gormley NJ, Bronstein AC, Rasimas JJ, et al. Rising incidence of intentional ingestion of ethanol-containing hand sanitizers. Critical Care Med 2012;40:290–4.
6. CDC. Hand hygiene saves lives: Patient admission video. http://www.cdc.gov/handhygiene/Patient_materials.html (Accessed April 8, 2016).
CLN's Patient Safety Focus is sponsored by ARUP Laboratories
