When it comes to persuading physicians to do things differently, there are two prevailing schools of thought. The fatalistic school holds that physicians are simply unmanageable. This perspective reflects the old—and sadly, too often accurate—stereotype of arrogant and intransigent physicians. To follow this approach means there is no choice but to defer to individual physician preferences. The other school of thought, which I’ll call the top-down school, acknowledges this stereotype and then asserts that to change physician behavior, it is necessary to take away their freedom of action. This school scoffs at weak behavioral interventions such as education, and promotes strong tactics such as forced clinical algorithms along with monetary rewards and penalties. MacArthur fellow and Harvard surgeon Atul Gawande’s famous proposal to run hospitals like Cheesecake Factory restaurants falls into this latter category (1). Unfortunately, neither the fatalistic nor the top-down approach present a fully satisfying theory of physician management, and both can bring negative consequences when applied broadly.
The problem with both approaches lies in the incredible complexity at the intersection of human biology and modern medical technology. Neither unassisted individual physicians nor administrators acting from a distance are fully capable of navigating this complexity alone. In Gawande’s Cheesecake Factory example, the limited number of inputs (ingredients, appliances, utensils, and the orderable options on the menu) can be controlled rigorously all the way through to the final product. In medicine, on the other hand, the primary inputs—patients and their diseases—are strikingly more complex. Each individual is different. Each disease presentation is different. Comorbidities are common. Every patient has different values and preferences for care. And great physicians customize care to individual patients to achieve superior outcomes.
Certainly, most factors in healthcare delivery can and should be standardized. But to become a great healthcare system, it’s also necessary to identify the factors that should remain flexible in order to support the work of of our best doctors. What we need, in other words, is a theory of active, engaged management that respects the professional role of physicians and takes full advantage of their education, skills, and ingenuity.
One useful tactic under this approach is nudging, i.e. steering physicians in the direction that we know is usually right, while still giving them freedom to deviate where appropriate. This requires engineering the information environment in which they act, such that usually correct actions become the default, and deviation requires a conscious choice. In more formal terms, nudging is an application of behavioral economics, which blends economics and psychology.
The book, Nudge, written in 2009 by two University of Chicago professors, popularized this concept (2). Classic economic theory holds that people will always act in their rational self interest. Psychology, on the other hand, knows that there are all kinds of reasons why people don’t, ranging from misperceptions to inertia. Over the past 2 decades, researchers have been studying practical ways to exploit these biases in order to steer people into changing their behavior.
For example, herd mentality is one common type of bias. Applying this to doctors, we see that they tend to adopt the practice styles of their more experienced peers. This can be a bad thing when those peers are wasteful or unsafe. But the herd mentality bias can be turned to advantage by identifying local physicians whose practice patterns are desirable and holding up their practice patterns as a standard. This creates the perception that these physicians are the primary peers, or “herd.”
In 2010, British Prime Minister David Cameron established a Behavioral Insights Team within his government. This body’s mandate is to use the principles of behavioral economics to influence the behavior of Britons in useful ways. For example, one of its most prominent experiments tackled the problem of citizens who didn’t pay their taxes on time. The British government already had a database that was used for sending out threatening reminder letters to delinquent citizens. But these letters didn’t seem to have much effect. So David Halpern, a former psychology professor at the University of Cambridge and the director of the Behavioral Insights Team, experimented with several alternative messages. Some letters cited the proportion of British taxpayers who paid on time. Others simply said that the majority of Britons in the recipients’ same income bracket had paid on time. Both messages turned out to have a significant positive impact on the rate of on-time payment (3).
A recent JAMA article described a randomized controlled trial of three behavioral interventions to nudge primary care doctors to reduce their use of antibiotics for acute respiratory tract infections (4). Most such infections are viral in origin, and the unnecessary use of antibiotics contributes to antibiotic resistance. One intervention, “suggested alternatives,” used popup messages within the electronic medical record. These messages recommended a non-antibiotic approach and facilitated ordering of applicable alternatives such as decongestants. A second, “peer comparison,” issued reports to physicians that compared their antibiotic ordering rates to their top-performing peers—notably, not the average of their peers. A third, “accountable justification,” required physicians to type in their reasons for deviating from the recommended therapy. All three interventions lowered the rate of inappropriate prescribing, and two of them achieved statistical significance. There were additive effects among the three, so that providing two or three interventions produced a bigger effect than any one alone. All three interventions respected physicians’ clinical judgment and allowed them to prescribe according to their judgment without penalty.
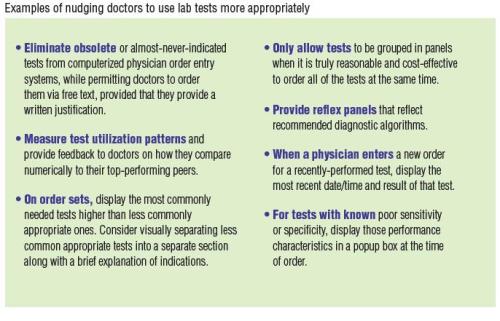
The direct implications of these experiments on lab utilization management are straightforward: we should provide alternative orders to commonly misordered tests; compare physicians’ ordering patterns to those of high-performing peers; and require written justification for orders that deviate from the standard recommendations. A less obvious implication is that these activities are better done in concert rather than in isolation. More broadly, the lesson is that in many use cases, hard controls may not be either necessary or even desirable for managing laboratory utilization.
If we are to solve the considerable challenges of achieving accountable care, it will require creative collaboration among all players in the healthcare system: clinicians, administrators, laboratory professionals, insurance companies, and others. This necessitates that each party bring out the best in the others. We need to be active and assertive in setting goals and holding each other accountable to those goals. But we also need to do this in ways that promote, rather than suppress, teamwork. Nudging can be a valuable tool in that it actively steers subjects in a particular direction, while preserving respect for their professional judgment.
References
1. Gawande A. Big med. New Yorker. August 13, 2012.
2. Thaler RH, Sunstein SR. Nudge: Improving decisions about health, wealth, and happiness. London: Penguin Books 2009.
3. Bennhold K. Britain’s ministry of nudges. New York Times. December 7, 2013.
4. Meeker D, Linder JA, Fox CR, et al. Effect of behavioral interventions on inappropriate antibiotic prescribing among primary care physicians: A randomized controlled trial. JAMA 2016;315(6):562–70.
Brian Jackson, MD, MS, is vice president and chief medical informatics officer at ARUP Laboratories, and an associate professor of clinical pathology at the University of Utah in Salt Lake City. +Email: [email protected]
CLN's Patient Safety Focus is sponsored by ARUP Laboratories
