Body fluids from individuals with possible Creutzfeldt-Jakob disease (CJD) present distinctive safety challenges for clinical laboratories. Sporadic, iatrogenic, and familial CJD (known collectively as classic CJD), along with variant CJD, kuru, Gerstmann-Sträussler-Scheinker, and fatal familial insomnia, are prion diseases, also known as transmissible spongiform encephalopathies. Prion diseases affect the central nervous system, and from the onset of symptoms follow a typically rapid progressive neurological decline. While prion diseases are rare, it is not uncommon for the most prevalent form—sporadic CJD—to be included in the differential diagnosis of individuals presenting with rapid cognitive decline. Thus, laboratories may deal with a significant number of possible CJD cases, and should have protocols in place to process specimens, even if a confirmatory diagnosis of CJD is made in only a fraction of these cases.
The Lab’s Role in Diagnosis
Laboratory protocols for handling specimens from individuals with possible, probable, and definitive cases of CJD are important to ensure timely and appropriate patient management. When the differential includes CJD, an attempt should be made to rule-in or out other causes of rapid neurological decline. Laboratories should be prepared to process blood and cerebrospinal fluid (CSF) specimens in such cases for routine analyses.
Definitive diagnosis requires identification of prion aggregates in brain tissue, which can be achieved by immunohistochemistry, a Western blot for proteinase K-resistant prions, and/or by the presence of prion fibrils. Thus, confirmatory diagnosis is typically achieved at autopsy. A probable diagnosis of CJD is supported by elevated concentration of 14-3-3 protein in CSF (a non-specific marker of neurodegeneration), EEG, and MRI findings. Thus, the laboratory may be required to process and send CSF samples to a prion surveillance center for 14-3-3 testing, as well as blood samples for sequencing of the PRNP gene (in inherited cases).
Processing Biofluids
Laboratories should follow standard protective measures when working with biofluids potentially containing abnormally folded prions, such as donning standard personal protective equipment (PPE); avoiding or minimizing the use of sharps; using single-use disposable items; and processing specimens to minimize formation of aerosols and droplets. An additional safety consideration is the use of single-use disposal PPE; otherwise, re-usable items must be either cleaned using prion-specific decontamination methods, or destroyed.
Blood. In experimental models, infectivity has been detected in the blood; however, there have been no cases of secondary transmission of classical CJD via blood product transfusions in humans. As such, blood has been classified, on epidemiological evidence by the World Health Organization (WHO), as containing “no detectible infectivity,” which means it can be processed by routine methods. Similarly, except for CSF, all other body fluids contain no infectivity and can be processed following standard procedures.
In contrast to classic CJD, there have been four cases of suspected secondary transmission of variant CJD via transfused blood products in the United Kingdom. Variant CJD, the prion disease associated with mad cow disease, is unique in its distribution of prion aggregates outside of the central nervous system, including the lymph nodes, spleen, and tonsils. For regions where variant CJD is a concern, laboratories should consult their regulatory agencies for further guidance.
CSF. Relative to highly infectious tissues of the brain, spinal cord, and eye, infectivity has been identified less often in CSF and is considered to have “low infectivity,” along with kidney, liver, and lung tissue. Since CSF can contain infectious material, WHO has recommended that analyses not be performed on automated equipment due to challenges associated with decontamination. Laboratories should perform a risk assessment of their CSF processes, and, if deemed necessary, consider using manual methods as an alternative to automated systems.
Decontamination
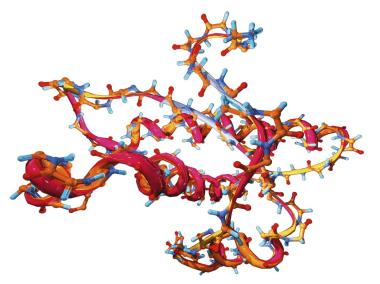
The infectious agent in prion disease is unlike any other infectious pathogen encountered in the laboratory; it is formed of misfolded and aggregated prion proteins. This aggregated proteinacious material forms the infectious unit, which is incredibly resilient to degradation. Moreover, in vitro studies have demonstrated that disrupting large aggregates into smaller aggregates increases cytotoxicity. Thus, if the aim is to abolish infectivity, all aggregates must be destroyed. Disinfectant procedures used for viral, bacterial, and fungal pathogens such as alcohol, boiling, formalin, dry heat (<300°C), autoclaving at 121°C for 15 minutes, and ionizing, ultraviolet, or microwave radiation, are either ineffective or variably effective against aggregated prions.
The only means to ensure no risk of residual infectious prions is to use disposable materials. This is not always practical, as, for instance, a biosafety cabinet cannot be discarded if there is a CSF spill in the hood. Fortunately, there are several protocols considered sufficient for decontamination. For surfaces and heat-sensitive instruments, such as a biosafety cabinet, WHO recommends flooding the surface with 2N NaOH or undiluted NaClO, letting stand for 1 hour, mopping up, and rinsing with water. If the surface cannot tolerate NaOH or NaClO, thorough cleaning will remove most infectivity by dilution. Laboratories may derive some additional benefit by using one of the partially effective methods discussed previously. Non-disposable heat-resistant items preferably should be immersed in 1N NaOH, heated in a gravity displacement autoclave at 121°C for 30 min, cleaned and rinsed in water, then sterilized by routine methods. WHO has outlined several alternate decontamination methods. Using disposable cover sheets is one simple solution to avoid contaminating work surfaces and associated lengthy decontamination procedures.
With standard PPE—augmented by a few additional safety measures and prion-specific decontamination procedures—laboratories can safely manage biofluid testing in cases of prion disease.
Mari DeMarco, PhD, DABCC, is a clinical chemist at St Paul’s Hospital and clinical assistant professor of pathology and laboratory medicine at the University of British Columbia in Vancouver. +Email: [email protected]