Solid cancer tumors typically are diagnosed, graded, and staged using tissue biopsy in which all or part of a neoplasm—usually the primary tumor—is removed for histological examination and genetic and molecular analysis. While tissue biopsy provides important diagnostic and therapeutic information, it has several inherent drawbacks that limit its clinical utility. To overcome these, new biopsy techniques are being developed and evaluated.
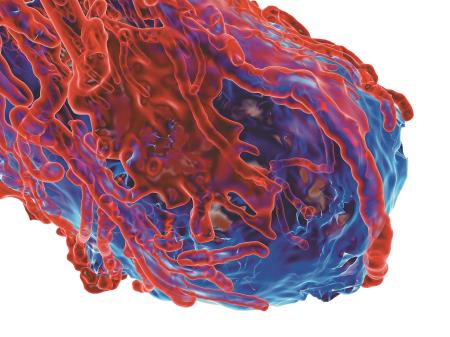
A particularly promising method is liquid biopsy, which exploits the presence of tumor cells in the bloodstream. As Bert Gold, PhD, FACMG, a staff scientist with the National Cancer Institute’s Center for Cancer Research explained, “Circulating tumor cells are cells of origin from a usually solid tumor that have gone into the general circulation and can be viewed in peripheral blood.” Enthusiasm for this approach reflects its potential to sidestep the limitations of tissue biopsy. For example, tissue biopsy is invasive, poses some risk to patients, and is often painful, slow, and costly, and therefore not practical for closely monitoring a patient’s disease progression and treatment response. In contrast, liquid biopsy requires only a simple blood draw; therefore, it poses little risk, and is quick, painless, and cost-effective. As such it may enable clinicians to closely monitor disease progression and treatment response in near real time without unduly burdening the patient.
Underscoring the significance of this capability, James Hicks, PhD, a research professor of biological sciences at the University of Southern California’s Institute for Convergent Science stated, “What’s important is following the [tumor’s] genotypic and phenotypic response to treatment, and being able to tell when and how the cancer might be becoming resistant or showing sensitivity to specific treatments.” Indeed, liquid biopsy may facilitate more personalized care for each patient.
CTC Isolation and Detection
The success of the liquid biopsy approach depends on isolation and detection of circulating tumor cells (CTCs), a challenging task given their rarity—about 1 to 10 CTCs per mL of whole blood. Numerous isolation and detection strategies are being developed and investigated for clinical use. In general, these isolate CTCs based on distinguishing biological and physical properties.
Biological strategies primarily use antibodies against tumor-specific cell surface antigens such as epithelial cell adhesion molecule (EpCAM) to identify CTCs. Typically these assays utilize antibody-coated magnetic beads that bind with the targeted antigen. Labeled CTCs are then removed from suspension with a magnet. An example of this type of immunomagnetic assay is the CellSearch system (Veridex, Johnson and Johnson) which is the only Food and Drug Administration–cleared CTC isolation system for CTC enumeration in whole blood in advanced breast, prostate, and colorectal cancers.
While simply enumerating CTCs in a blood sample may not seem to provide significant clinical information, Gold begged to differ. “For breast, prostate, and colon cancers it is now clear that the number of CTCs is a good prognostic predictor of survival,” he explained.
Physical strategies use cell properties such as size, density, and deformability to isolate CTCs. These systems, like ISET and ScreenCell, often employ membranous filtration devices to sort cells according to size. Other methods, such as JETTATM, employ size- and deformability-based CTC isolation. Still other CTC isolation and detection platforms, like CTC-iChip and Isoflux, combine immunomagnetic enrichment with microfluidics techniques that use physical properties to separate and sort cells.
Molecular assays are also being developed that isolate CTCs based on gene expression which is analyzed using total CTC RNA and reverse transcription polymerase chain reaction techniques to amplify tumor- and epithelial-specific markers.
The Epic Sciences High Definition CTC (HD-CTC) assay employs a novel strategy, avoiding affinity-based methods that, as Hicks noted, can bias results. “Almost all [CTC isolation and detection] methods depend on your prior knowledge of what cells to select for; you need a criterion. As soon as you impose a criterion you’re eliminating whatever cells there might be that you don’t know about but which might be important for that disease,” he explained. Indeed, antibody-based methods can miss CTCs expressing low levels of select tumor markers such as EpCAM. To eliminate this weakness, HD-CTC maintains all cells without enriching the samples with particular tumor markers. The assay measures protein expression, and interrogates genomic abnormalities in CTCs for more than 20 different cancer types.
CTC isolation, detection, and molecular characterization systems are being investigated not only in breast, prostate, and colon cancers but also pancreas, lung, skin, and head and neck cancers, among others. Currently, clinical use of isolation and detection technology is limited to enumeration of CTCs. However, CTC number has been shown to correlate with disease severity in at least some cancer types. For example, breast, prostate, and colorectal cancer patients with fewer CTCs in their blood had longer survival times than those with more CTCs. CTC number has also been shown to predict survival in breast and prostate cancers, and to be a prognostic predictor of overall survival for malignant melanoma. Analyzing CTC genetic mutations is also helping to identify biomarkers for disease progression rate and drug response in various types of cancer.
Clinical Adoption of CTC Analysis
Before CTC testing becomes part of routine clinical practice, many questions need to be answered and challenges overcome. Perhaps foremost among these is the issue of assay accuracy and consistency. There is evidence suggesting that the results of CTC analysis vary according to the isolation and detection system used. Accordingly, the sensitivity and specificity of these technologies need to be optimized to eliminate any selection bias. To this end, CTC phenotypes must be characterized more thoroughly, and all phases of CTC isolation and detection standardized and subjected to quality control, according to experts.
In addition, the potential of CTCs to serve as biomarkers needs to be validated. This will require determining the extent to which CTCs represent their tumor of origin, clarifying the relationship between tumor burden and CTC number, and defining the prognostic significance of CTC detection. Also, more extensive molecular characterization of CTCs is needed to elucidate mechanisms of drug resistance and metastasis, and to personalize anti-metastatic therapies. To this point, Hicks observed, “It’s going to take a lot more work to figure out exactly what a blood sample is telling us about the thing we really care about, which is metastasis.”
There also needs to be thorough investigation of the relative benefits of CTC versus circulating tumor-derived DNA (cfDNA) analysis. Dennis Lo, MD, PhD, professor of medicine and chemical pathology at the Chinese University of Hong Kong, and director of the Li Ka Shing Institute of Health Sciences is a pioneer in the field of cfDNA research. Regarding the clinical utility of CTC and cfDNA analysis he stated, “Data from a number of groups seem to indicate that the fractional concentration of tumor-derived cfDNA in plasma is higher than fractional concentrations of CTCs in whole blood. Hence, cfDNA can probably be analyzed more easily and [inexpensively] than CTCs.” Others, such as Hicks, envision CTC, cfDNA, and cfRNA analyses as complimentary approaches that might be employed in conjunction. Each method needs to be investigated further and validated before use in the clinical setting.
While remarkable progress is being made in elucidating CTC biology, and numerous groups are aggressively pursuing development of clinical CTC assays, fundamental questions must be answered before CTC analysis can be adopted into routine practice. As Gold put it, “We can’t say for certain that CTCs are not good predictors of tumor sensitivity to anti-cancer drugs, but we can’t say they are good predictors either. We’re sort of stuck until a bunch more research is funded and done.”
Curtis Balmer, PhD, is a freelance science writer in Potomac Falls, Virginia.
+Email: [email protected]