
Designer drugs continue to make headlines in the U.S. and abroad. In one recent large-scale incident, New York City officials shut down the 2013 Electric Zoo music festival on Labor Day weekend after two concertgoers died and several others were hospitalized from an apparent ecstasy overdose. Investigators later discovered that the usual psychoactive substance found in ecstasy—3,4-methylenedioxy-N-methylamphetamine (MDMA)—had been replaced or combined with a more potent synthetic designer stimulant known as methylone, one of many substances found in a new breed of stimulant/hallucinogenic designer drugs called bath salts (1). Bath salts are rising in popularity along with a wave of other new designer drugs like synthetic cannabinoids and opioids. Today, 10% of U.S. high school seniors admit to recent use of synthetic cannabinoids (2).
Given the prevalence of and public alarm about designer drugs, clinical laboratories face a formidable challenge in validating testing platforms for bath salts and other emerging drugs. Unfortunately, information gaps and a lack of appropriate analytical reference standards make it difficult for a laboratory to meet stringent accreditation requirements. In this article, we review the complex nomenclature and drug composition encountered with bath salt formulations, along with available pharmacology, pharmacokinetics, and testing information. Together, this information highlights challenges that clinical laboratories face and provides strategies for overcoming these barriers.
What Are Bath Salts?
In illicit designer drug markets, bath salts are far removed from the ordinary salt crystals purchased for a relaxing spa. These synthetic drugs are formulated for their potent stimulant and hallucinogenic properties. As might be expected, there is no quality control in the manufacturing of bath salts. Dosages, formulations, and drug mixtures vary from product to product and from batch to batch, and adulterants ranging from caffeine to methamphetamine are common. Adding to the complexity of the problem, bath salts are found under a variety of labels, packaging, and physical formulations, such as a white powder, tablets, or liquid. As a result, users never know exactly what they are about to consume, and an unusual assortment of disingenuous labels like plant food, insect repellant, or even "Vanilla Sky" and "Meow Meow" add further confusion—especially for new drug users, adolescents, and parents.
Figure 1
Chemical structures of common bath salt stimulant and
hallucinogenic compounds
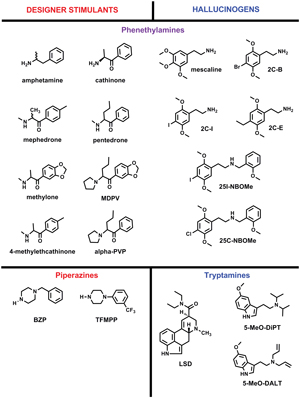
Bath salts contain several psychoactive substances thought to have stimulant and/or hallucinogenic properties. Bath salts possessing primarily stimulant-like properties are commonly considered phenethylamine or piperazine analogs, which have a similar chemical structure as the well characterized stimulants cathinone, amphetamine, or benzylpiperazine (BZP) (Figure 1). Winstock et al. recently surveyed patrons of night clubs in the U.K. and found that nearly 50% used the cathinone analogs mephedrone and/or methylone (Figure 1) (3). Similar to other studies, the authors tracked for nearly 4 years the prevalence of designer drugs seized by law enforcement in Arkansas (3, 4). Analysis of 489 items identified the six most common psychoactive drugs as MDPV (methylenedioxypyrovalerone), 4-MEC (4-methyl-N-ethylcathinone), pentedrone (2-(methylamino)-1-phenylpentan-1-one), α-PVP (α-pyrrolidinopentiophenone), BZP, and TFMPP (3-trifluoromethyl-phenylpiperazine). These substances were formulated as powders, tablets, and capsules (Figure 2).
Figure 2
Analysis of 489 bath salt cases demonstrates the prevalence of stimulant and hallucinogenic compounds in tables, capsules, powder, and blotter paper seized by Arkansas law enforcement during a 4-year period.

While rare, designer stimulants are also found in plant material and smoked like K2 synthetic cannabinoids. Also, bath salt compounds are commonly found as mixes containing other synthetic drugs or illicit substances, like methamphetamine, ketamine, and MDMA (5). Of the total 489 items analyzed in Figure 2, only 189 (39%) contained a single compound and more than 100 unique drug mixtures were identified. These dangerous drug combinations pose significant clinical and analytical challenges.
Bath salts can also contain potent hallucinogenic drugs biochemically characterized as analogs of mescaline or LSD (Figure 1). Mescaline is a natural hallucinogenic phenethylamine compound found in the peyote cactus (Lophophora williamsii), whereas tryptamine hallucinogens are similar to LSD. Alexander Shulgin is well known for his books PiHKAL and TiHKAL, which provide detailed synthesis procedures and a firsthand account of the pharmacological effects (6, 7). These hallucinogens are also formulated as powders, capsules, and tablets and may be used to lace blotter paper (5). Marketing names vary greatly from "smiles," "7th-heaven," and "Foxy"to an abbreviated biochemical name like 2C-B or 2C-E. The LSD analog 25I-NBOMe was the most common hallucinogen detected as part of our 4-year surveillance program in Arkansas, in which 10% of the pills, tablets, capsules, and blotter paper contained 25I-NBOMe (Figure 2).
Pharmacology
When insufflated, ingested, or injected, bath salts have dire toxicological consequences. In general, these drugs modulate neurotransmitter release and/or neurotransmitter reuptake mechanisms, but the molecular mechanisms underlying human toxicity remain to be determined. The toxicology of the synthetic cathinones and piperazines is similar to MDMA, with most substances inhibiting re-uptake of dopamine and norepinephrine through inhibition of the monoamine uptake transporters. Serotonin levels also may be modulated due to inhibition of reuptake (8–10). On the other hand, the molecular mechanism of tryptamine and phenylethylamine hallucinogenic analogs found in bath salts, such as 5-MeO-DALT and the 2C compounds, are probably mediated through agonistic action at several serotonin receptors and ion channels (11–13).
The physical and neurological effects of bath salts can be extreme, debilitating, and even fatal (15, 18, 19). The toxicodynamics and toxicokinetics of the bath salts are unknown in humans, but animal studies are starting to emerge (14). Clinical reports demonstrate that the adverse effects of bath salts are similar to other stimulants, like MDMA. For example, multiple case reports indicate tachycardia, agitation, hyperthermia, hypertension (early on presentation), and confusion (15). Symptoms can be extreme, such as myocardial infarction in teens, brain swelling, and renal failure (15). Likewise, the adverse effects of the hallucinogen 25I-NBOMe commonly include tachycardia, agitation, visual and audio hallucinations, hypertension, and seizures (16, 17). In an extreme example, an individual who ingested the hallucinogen 2C-B experienced progressive encephalopathy and paralysis that did not improve over a 6 month period (18).
The Law
In the United States, most drugs sold as bath salts are listed in Schedule I of the Controlled Substances Act or regulated through analog law provisions (20, 21). Most state and federal analog provisions in the U.S. require structural and pharmacological comparison. Many other countries, particularly throughout Europe, regulate the sale and distribution of bath salts. Unfortunately, the availability of these drugs online and their low cost limit the effectiveness of regulation. For example, bulk amounts of methylone and 2C-B (500 g) can be purchased online for around $2.50 per 1 gram of pure compound, whereas a normal dose of methylone is 100–250 mg and 2C-B is 15–25 mg (22, 23, 24).
Testing for Bath Salts
Several contract and research testing laboratories have used liquid chromatography/tandem mass spectrometry (LC-MS/MS), gas chromatography/mass spectrometry (GC-MS), and liquid chromatography/time-of-flight mass spectrometry (LC/TOF-MS) testing platforms to develop qualitative and quantitative testing procedures for assaying bath salts in blood, urine, serum, and plasma (25–27). However, analytical capacity is still limited for several of the phenethylamine and tryptamine analogs listed in Figure 1. Further complicating matters is the expanding list of emerging drugs. Methodology also can become complex; for example, polarity switching is often required in mass spectrometry methods (14). While laboratories struggle to keep pace with the proliferating new bath salt compounds, users continue to evade detection in standardized drug tests.
Responding to the Challenge
Whether the compound is a phenethylamine, piperazine, or tryptamine, bath salts are gaining popularity and represent a major challenge for healthcare professionals, public health officials, clinical laboratories, and law enforcement. The easy availability of these drugs online has enabled users to evade attempts at regulation. Although the biomedical community is responding, educational efforts aimed at local communities and healthcare professionals are still necessary to demonstrate the toxic nature of these stimulant and/or hallucinogenic substances. The effects in humans are difficult to predict and more studies are required. Since chemical compositions continually change to purposely avoid detection and regulation, it is difficult to determine what drugs need to be studied. Seemingly, researchers are always one step behind.
Since most, if not all, synthetic stimulants and hallucinogens are not detected using routine clinical toxicology tests, healthcare providers and clinical laboratories should be aware of potential toxicity of these compounds even with negative test results. Screening methods for bath salts are not widely available, and several designer stimulants cross-react in amphetamine immunoassays (28). Thus, designer stimulant use should be considered in clinical cases where amphetamine exposure is suggested by positive immunoassay but mass spectral confirmation fails.
The growing abuse of bath salts highlights the need for clinical laboratories to develop robust methodologies that keep pace with new drugs as they keep emerging. This is a lofty goal, but with open communication among laboratories and commercial vendors, success may not be as far off as it seems. The problems associated with designer drug testing are here to stay and the demands on clinical laboratories will only increase, especially as reports of morbidity and mortality drive public concern.
REFERENCES
- The New York Times. Overdoses of “Molly” led to Electric Zoo deaths. http://artsbeat.blogs.nytimes.com/2013/09/12/overdoses-of-molly-led-to-electric-zoo-deaths/?_r=0 (Accessed October 2013).
- Vandrey R, Dunn KE, Fry JA, et al. A survey study to characterize use of Spice products (synthetic cannabinoids). Drug Alcohol Depend 2012;120:238–41.
- Winstock AR, Mitcheson LR, Deluca P, et al. Mephedrone, new kid for the chop? Addiction 2011;106:154–61.
- Leffler AM, Smith PB, de Armas A, et al. The analytical investigation of synthetic street drugs containing cathinone analogs. [Epub ahead of print] Forensic Sci Int October 22, 2013 as http://dx.doi.org/10.1016/j.forsciint.2013.08.021.
- Seely KA, Patton AL, Moran CL, et al. Forensic investigation of K2, Spice, and "bath salt" commercial preparations: A three-year study of new designer drug products containing synthetic cannabinoid, stimulant, and hallucinogenic compounds. [Epub ahead of print] Forensic Sci Int October 22, 2013 as http://dx.doi.org/10.1016/j.forsciint.2013.10.002.
- Shulgin AT, Shulgin A. Pihkal: A Chemical Love Story. California: Transform Press 1991.
- Shulgin AT, Shulgin A. Tihkal: A Continuation. California: Transform Press 1997.
- Baumann MH, Ayestas MA, Jr., Partilla JS, et al. The designer methcathinone analogs, mephedrone and methylone, are substrates for monoamine transporters in brain tissue. Neuropsychopharmacology 2012;37:1192–203.
- Baumann MH, Partilla JS, Lehner KR. Psychoactive bath salts: Not so soothing. Eur J Pharmacol 2013;698:1–5.
- Lehner KR, Baumann MH. Psychoactive "bath salts": Compounds, mechanisms, and toxicities. Neuropsychopharmacology 2013;38:243–4.
- Brandt SD, Tearavarich R, Dempster N, et al. Synthesis and characterization of 5-methoxy-2-methyl-N,N-dialkylated tryptamines. Drug Test Anal 2012;4:24–32.
- Hill SL, Thomas SH. Clinical toxicology of newer recreational drugs. Clin Toxicol (Phila) 2011;49:705–19.
- Rose SR, Poklis JL, Poklis A. A case of 25I-NBOMe (25-I) intoxication: A new potent 5-HT2A agonist designer drug. Clin Toxicol (Phila) 2013;51:174–7.
- Lopez-Arnau R, Martinez-Clemente J, Carbo ML, et al. An integrated pharmacokinetic and pharmacodynamic study of a new drug of abuse, methylone, a synthetic cathinone sold as bath salts. [Epub ahead of print] Prog Neuropsychopharmacol Biol Psychiatry April 18, 2013 as doi:10.1016/j.pnpbp.2013.04.007.
- Miotto K, Striebel J, Cho AK, et al. Clinical and pharmacological aspects of bath salt use: A review of the literature and case reports. Drug Alcohol Depend 2013;132:1–12.
- Hill SL, Doris T, Gurung S, et al. Severe clinical toxicity associated with analytically confirmed recreational use of 25I-NBOMe: Case series. Clin Toxicol (Phila) 2013;51:487–92.
- Smolinske SC, Rastogi R, Schenkel S. Foxy methoxy: A new drug of abuse. J Med Toxicol 2005;1:22–5.
- Ambrose JB, Bennett HD, Lee HS, et al. Cerebral vasculopathy after 4-bromo-2,5-dimethoxyphenethylamine ingestion. Neurologist 2010;16:199–202.
- Tanaka E, Kamata T, Katagi M, et al. A fatal poisoning with 5-methoxy-N,N-diisopropyltryptamine, Foxy. Forensic Sci Int 2006;163:152–4.
- Synthetic Drug Abuse Prevention Act. 2012. In: Justice Do (ed) XI, vol 112-114.
- Schedules of Controlled Substances. CP 1308. 2011;76:11075–8.
- Legal Powder Ltd. http://legalpowder.cn.com/home.html (Accessed October 2013).
- Erowid. Methylone Dosage. http://www.erowid.org/chemicals/methylone/methylone_dose.shtml (Accessed October 2013).
- Erowid. 2C-B Dose. http://www.erowid.org/chemicals/2cb/2cb_dose.shtml (Accessed October 2013).
- Redwood Toxicology Laboratory. Designer Stimulant Test. https://www.redwoodtoxicology.com/services/designer_stimulant_testing (Accessed October 2013).
- NMS Labs. Comprehensive Stimulants and Hallucinogens Panel, Liquid Test. http://www.nmslabs.com/tests/Comprehensive-Stimulants-and-Hallucinogens-Panel--Liquid/7210LI (Accessed October 2013).
- Laboratory Corporation of America. Mephedrone, MDPV, and Methylone, Urine. https://www.labcorp.com/ (Accessed October 2013).
- Petrie M, Lynch KL, Ekins S, et al. Cross-reactivity studies and predictive modeling of "bath salts" and other amphetamine-type stimulants with amphetamine screening immunoassays. Clin Toxicol (Phila) 2013;51:83–91.
 Kathryn A. Seely, PhD, is laboratory manager of Chemical Terrorism at the Arkansas Public Health Laboratory, Arkansas Department of Health. Email: [email protected]
Kathryn A. Seely, PhD, is laboratory manager of Chemical Terrorism at the Arkansas Public Health Laboratory, Arkansas Department of Health. Email: [email protected]
 Jeffery H. Moran, PhD, is branch chief of Environmental Chemistry at the Arkansas Public Health Laboratory, Arkansas Department of Health and assistant professor in the College of Medicine, University of Arkansas for Medical Sciences. Email: [email protected]
Jeffery H. Moran, PhD, is branch chief of Environmental Chemistry at the Arkansas Public Health Laboratory, Arkansas Department of Health and assistant professor in the College of Medicine, University of Arkansas for Medical Sciences. Email: [email protected]