
Mike Astion, MD, PhD
Editor, Patient Safety Focus
Medical Director, Department of Laboratories
Seattle Children’s Hospital
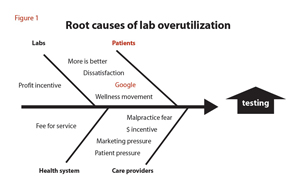
The causes of ordering too many lab tests are diverse and complex. However, the consequences are only too clear: waste of scarce healthcare resources, and potential for real patient harm. On the patient side, the Googlefication of healthcare raises alarm about problems that might be better left unexamined. What was once a runny nose requiring no doctor visit now becomes, with just a few key clicks, an opportunity to worry about—and demand testing for—the allergens, viruses, bacteria, autoimmune diseases, nutritional deficiencies, and toxins that could be causing it. For the worried well, the Internet can turn a bout of fatigue into an opportunity to think about poisonings, malnutrition, and cancer.
Too often, social media exacerbate the problem because they allow the worried well to broadcast their concerns and find an exceptional case that confirms their worst fears—the friend, who has a friend, whose brother thought he had a common cold but turned out to have a rare and fatal disease. Unfortunately, the most common ambulatory complaints, including headache, backache, stomach pain, anxiety, and depressed mood, have very little useful lab testing associated with them. In fact, lab testing in the context of these common ambulatory complaints is as likely to confuse as to inform.
Patients don’t bear all the blame, however. The U.S. healthcare industry promotes overtesting in outpatients because it is primarily based on a fee-for-service system. Even labs play a role in overutilization because, to the extent that they participate in fee-for-service medicine, overutilization can provide significant financial benefits. Physicians have their own reasons for testing too frequently in the outpatient setting, including practicing defensive medicine and the inability to resist patient and marketing pressures.
In addition, some physicians use lab testing to differentiate themselves in the healthcare marketplace. For example, some anti-aging specialists offer large testing panels because they believe that these panels can guide interventions to slow down aging. Similarly, some providers order alternative testing for infectious diseases under the assumption that these tests reveal stealth infections that are the basis of a number of ailments.
Combating Overutilization
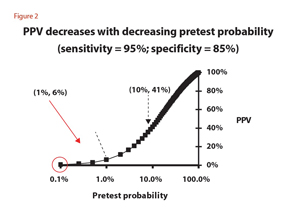
Test ordering errors increase the likelihood of test interpretation errors. But the consequences of this fact are not always intuitive. Figure 2 illustrates overutilization with a graph of positive predictive value (PPV) versus pretest probability. Pretest probability is the likelihood that a patient has the disease being tested for, and it is based on the patient’s history and physical. For example, a 40-year old woman with a history of back pain who wakes up with a headache twice per month has a low pretest probability that the headache is being caused by heavy metal poisoning, an autoantibody disease, a nutritional deficiency, or a stealth virus.
PPV is the probability that a positive test result indicates that the patient has the disease for which the test is being performed. A positive result refers to a result outside a reference range or above a cutoff value. In the figure, a test was chosen that had a specificity of 85% and a sensitivity of 95%. This would be the typical performance range for a number of tests including the antinuclear antibody (ANA) test, or individual tests for specific allergies or infectious diseases.
As the graph shows, the pretest probability very strongly influences the PPV. The diagnostic utility of a positive test is particularly poor when the pretest probability is low. In this example, it means that at a pretest probability of 1%, the probability that a positive result indicates the presence of the disease is only 6%. In other words, the odds strongly favor the patient not having the disease despite testing positive for it.
In my experience, both patients and physicians do not understand just how poorly tests perform diagnostically in the low pretest probability range. Thus, in our example, if the woman with a headache demands an ANA test and receives a positive test result, it is likely to be a false positive. That is why it would have been better to not test.
False positives are due to a variety of causes including overlap of the diseased and healthy state, lab errors, and lab interferences. A false positive result is often not believed by the worried well and this disbelief can lead to a medical misadventure of additional tests, misdiagnosis, and mistreatment. Today, it is the rare person who does not know a friend or relative who has gone on a testing-based misadventure. The relationships between pretest probability and PPV shown in figure 2 explain why testing too frequently in the ambulatory setting is a significant contributor to diagnostic error. Patients and physicians can avoid this false diagnosis problem by only undergoing or ordering testing when two conditions are met: 1) an actual lab test exists for the disease that is suspected, and 2) the pretest probability of disease is sufficient to allow a meaningful interpretation of a positive result. In the majority of medical encounters, this means that the patient will need to have signs, symptoms, family history, or personal history that suggests the disease has a reasonable likelihood of being present.
It is especially important to avoid testing in the ambulatory setting, where the pretest probability is low. Usually, testing will do more harm than good when the pretest probability of the disease being tested is 1% or below, and this is even the case for tests with sensitivity and specificity above 95%.
Further Reading
- Welch HG, Schwartz L, Woloshin S. Overdiagnosed: Making people sick in the pursuit of health. Boston: Beacon Press 2011.
- Moynihan R, Doust J, Henry D. Preventing overdiagnosis: How to stop harming the healthy. BMJ 2012;344:e3502. doi:10.1136/bmj.e3502.
- VassarStats: Website for statistical computation. Predictive values and likelihood ratios. http://vassarstats.net/clin2.html (Accessed November 27, 2013).