
Vitamin D arguably is one of the most intensely investigated nutrients of the 21st Century, the subject of at least 25,000 scientific articles since 2000. Experts largely agree that this fat-soluble prohormone is vital to bone health. Beyond that, however, interpretations of the evidence about vitamin D diverge sharply. In which biological processes does it play an important role? What are the proper intake amounts? How should deficiency, insufficiency, sufficiency, and toxicity be defined? Answers to these and other questions vary, sometimes considerably, depending on who is giving them. The good news is a major clinical trial now in progress could bring clarity to these uncertainties within the next few years. In the meantime, laboratorians caught in the crossfire of conflicting positions should keep apprised of ongoing research, remain a resource for clinicians, and ensure their vitamin D assays are as robust as possible, experts advise. AACC's Annual Meeting in Houston will provide lab professionals several opportunities to learn about the latest vitamin D-related evidence and testing technologies, including a plenary session, "The Vitamin D Debate," on Tuesday, July 30.
"Vitamin D has been a hot topic because there is debate on both ends of the spectrum. Some people are talking about its non-skeletal benefits and others are not that excited about its non-skeletal benefits, so there is not a consensus," said Muhammad Amer, MD, MHS, FACP, an assistant professor of medicine at Johns Hopkins University School of Medicine in Baltimore. "It's really a work in progress, unlike, for example, vitamins E and A, where we do not see any substantial change in terms of reported clinical outcomes such as cardiovascular health or all-cause mortality. With vitamin D there's no consensus just because of the nature of the existing data we have. But we're slowly and steadily heading in that direction and I would hope we have this sorted out relatively soon."
What's the Evidence?
How did the sunshine vitamin come to be so controversial? It was long understood to be available from both sunlight and dietary sources and not a vitamin in the classic sense of a nutrient the body needs in small amounts but can't make on its own. A series of discoveries dating from the 1960s establishing vitamin D as part of a tightly regulated endocrine system involving the liver, kidneys, and parathyroid glands as well as multiple target organs spurred interest in the potential effect it might have throughout the body. A spate of mostly observational studies that reported associations between vitamin D levels and a wide variety of diseases seemed to reinforce this notion.
Higher steady-state levels of vitamin D have been linked to cardiovascular, brain, musculoskeletal, periodontal, skin, respiratory and eye health, and to cancer prevention—particularly breast, colorectal, and prostate. Epidemiologic studies also have pointed to a connection between sunlight exposure, a surrogate for measuring vitamin D levels, and diseases such as multiple sclerosis and type 1 diabetes, with individuals living closer to the equator where the sun's ultraviolet rays are stronger having a lower incidence of these conditions in comparison to those at higher latitudes.
Many of these findings made their way into the media, and soon vitamin D was a hot topic on the airways, and in hallway conversations and doctors' offices. Laboratorians know all too well that the volume of vitamin D testing, once modest, skyrocketed throughout the 2000s. "The lay press, constantly publishing on all these new association studies, was driving this. Patients would go to doctors and say ‘please check my blood level,'" explained Michael F. Holick, PhD, MD. "Well, doctors would do it, then find patients were vitamin D-deficient. A light went off in their heads and now doctors are ordering it in all their patients. The 25-hydroxyvitamin D [25(OH)D] assay is the most-ordered esoteric test in the U.S., way above testosterone, estrogen, or anything else." A long-time vitamin D researcher, Holick is a professor of medicine, physiology, and biophysics at Boston University School of Medicine.
Setting New Daily Requirements
Amidst the testing bonanza, uncertainty has lingered about how much vitamin D is necessary as well as what levels most people should be aiming to maintain. In light of these questions and both public and scientific interest, the Institute of Medicine (IOM) in collaboration with Health Canada reviewed the evidence and in 2010 issued for both vitamin D and calcium updated daily reference intakes (DRIs), the amounts needed to meet the nutritional requirements of at least 97.5% of the population.
The panel, comprised of nutritionists and physicians from the U.S. and Canada, suggested that children age 1 or older and adults up to age 70 need 600 international units (IUs) of vitamin D per day to maintain bone health, and that adults age 71 and older need up to 800 IUs per day. These recommendations effectively tripled DRIs set in 1997 by the same panel with different members. The committee also issued recommended upper intake levels (ULs) ranging from 1,000 IUs per day for babies less than 6 months old to 4,000 IUs per day for children age 9 or older and all adults.
How Much Is Sufficient?
Even though these findings reflected a review of nearly 1,000 studies as well as testimony from scientists and stakeholders, they disappointed some in the vitamin D community. Scientists not on the panel had several issues with its conclusions. Two of the most significant, because they influenced the panel's other recommendations, were its assessment of the prevalence of vitamin D deficiency and the definitions it used for deficiency and sufficiency.
The IOM committee found that blood levels of 20 ng/mL would be sufficient for nearly all Americans and Canadians. Further, while the committee concluded from national surveys that average vitamin D intake is below this median requirement, it also determined that the majority of North Americans are receiving adequate vitamin D from sun exposure.
Other groups evaluated this evidence and reached different conclusions (see Table, below). For example, the Endocrine Society, in its 2011 clinical practice guidelines on the evaluation, treatment, and prevention of vitamin D deficiency, defined vitamin D deficiency as 20 ng/mL, and insufficiency as 21–29 ng/mL. This panel set a target of 30 ng/mL for vitamin D sufficiency, and determined that most of the population is at risk for deficiency. Based on these definitions and its assessment of the prevalence of deficiency, the Endocrine Society set higher DRIs for both sexes and all life stages. For infants and children up to age 18, it recommended 600–1,000 IUs per day, and for adults age 18 or older, the panel called for 1,500–2,000 per day.
Holick, who chaired the Endocrine Society panel, explained how these two expert bodies arrived at different recommendations. "The IOM used a population model and they made the assumption that most children and adults in the U.S. are vitamin D sufficient. But the Endocrine Society used a medical model to provide physicians and healthcare professionals with advice on how to treat and prevent vitamin D deficiency," he said. "Our goal had never been to provide recommendations for the population at large. But we did make those recommendations for the population that was at risk and we thought that essentially most of the population was at risk." Holick also served on the 1997 IOM panel.
|
Vitamin D Daily Requirements
Who Recommends What?
Disparities in recommended intake levels of vitamin D have created confusion for both physicians and patients.
|
| Life Stage |
International Units/ Day |
Institute
of Medicine |
Endocrine
Society |
Vitamin D
Council |
| Infants |
600 |
600–1,000 |
1,000 |
| Children |
600 |
600–1,000 |
1,000* |
| Women |
| 18–70 |
600 |
1,500–2,000 |
5,000 |
| >70 |
800 |
1,500–2,000 |
5,000 |
| Pregnant |
600 |
600–2,000 |
5,000 |
| Lactating |
600 |
600–2,000 |
5,000 |
| Men |
| 18–70 |
600 |
1,500–2,000 |
5,000 |
| >70 |
800 |
1,500–2,000 |
5,000 |
| Upper Intake Level |
| Infants |
| 0–6 months |
1,000 |
2,000 |
2,000 |
| 6–12 months |
1,500 |
2,000 |
2,000 |
| Children |
| 1–3 years |
2,500 |
4,000 |
2,000* |
| 4–8 years |
3,000 |
4,000 |
2,000* |
| 9–18 years |
4,000 |
4,000 |
2,000* |
| Adults |
4,000 |
4,000** |
10,000 |
*Per 25 lbs. body weight.
**Largest recommended dose without medical supervision. With medical supervision, upper intake level rises to 10,000. |
Testing Challenges
Of particular significance to laboratorians, the IOM panel observed that lab cutpoints for sufficiency and deficiency have "not been set based on rigorous scientific studies and no central authority has determined which cutpoints to use." The committee went on to note that an individual could be declared vitamin D deficient or sufficient depending on which lab performs the test. The panel also suggested the number of people with vitamin D deficiency could be overstated because many labs appear to be using higher cutpoints than those the committee recommended.
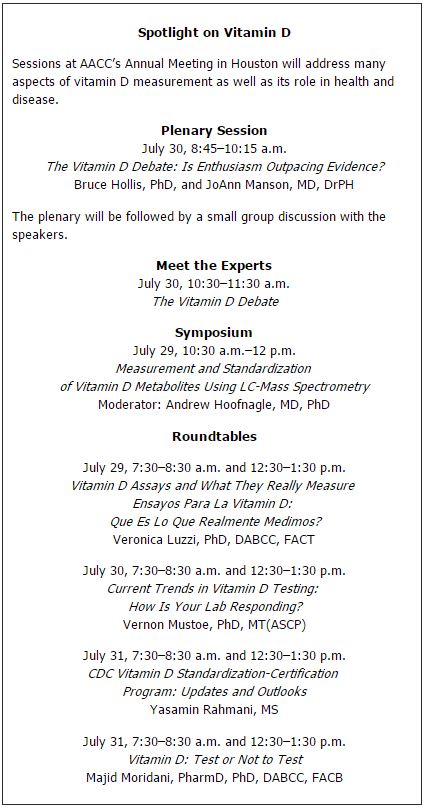
Holick agreed that testing variabilities continue to hamper the field, and indeed, a major initiative of the National Institutes of Health's Office of Dietary Supplements, the Vitamin D Standardization Program (VDSP), aims to improve lab measurements of vitamin D status in national health surveys. In addition, the Centers for Disease Control and Prevention's Hormone Standardization Program has started an initiative to improve the accuracy of vitamin D testing. Both these programs will be the subject of CLN's Series Article in August. Several sessions at the AACC Annual Meeting this month in Houston also will tackle various aspects of vitamin D testing, including a plenary session on the evidence about vitamin D as well as presentations on the VDSP and lab measurement issues. (See a list of these program offerings, below.)
Healthy Bones and More?
Another source of contention for observers of the IOM panel was that this body found evidence for vitamin D's role in promoting skeletal growth and maintenance, but not its many other purported health benefits. Panelist JoAnn Manson, MD, DrPH, elaborated on the committee's review process.
"We did a very comprehensive and rigorous review of the evidence, including our own internal review of close to 1,000 studies looking at many diseases and health outcomes, as well as considering the results of a systematic review sponsored by the Agency for Healthcare Research and Quality. In general we concluded that the evidence that vitamin D has health benefits pertain predominantly to bone health," she explained. "We felt that some of the evidence about other health outcomes was promising but remained inconsistent and inconclusive. In particular there wasn't clear evidence for a cause and effect relationship. There were many observational studies that suggested a possible correlation between a low vitamin D level and several negative health outcomes, but it's important to note that correlation does not prove causation." Manson is chief of the division of preventive medicine at Brigham and Women's Hospital and a professor of medicine at Harvard Medical School in Boston.
Among the researchers who took exception to the panel's findings was Bruce Hollis, PhD, a professor of pediatrics at the Medical University of South Carolina in Charleston. "Basically their recommendations were based along the lines of skeletal involvement and talk very little about anything else. The IOM committee made the decision that if a vitamin D study wasn't a randomized controlled trial, the results would not be accepted. But the truth is there have been small randomized controlled trials involving vitamin D and cancer, diabetes, and cardiovascular disease, some of them quite positive," he contended. A well-known vitamin D researcher, Hollis developed and received royalties for a vitamin D immunoassay method used by DiaSorin.
Manson expounded on the many factors that caused the panel to rely on the highest level of evidence, randomized controlled trials. Obese individuals tend to have lower vitamin D levels because this fat-soluble vitamin is sequestered in fat tissue, she noted. In addition, physically active study subjects might be outside more and have greater sun exposure, thereby synthesizing more vitamin D, but their health benefits could be from exercise itself rather than vitamin D. Individuals with dark skin don't synthesize vitamin D as efficiently as others, and African-Americans in particular tend to have lower intake from food sources, making their overall levels lower.
"Those are just a few of the major potential confounders of this relationship, and it's very difficult to adjust well for those variables. That's why randomized controlled trials are so important, as they balance out these other factors," Manson explained. "It's really amazing that in 2013 we don't have any large-scale, randomized controlled trials that already are completed to provide these answers."
Too Much of a Good Thing?
Hollis also chafed at the IOM's UL recommendations and its conclusion that risk for harm increases after intakes exceed 4,000 IUs per day. The Endocrine Society also recommended a UL of 4,000 IUs per day without medical supervision for all individuals age 9 or older. However, it advised that considerably larger doses up to 10,000 IUs per day for adults might be necessary to remedy deficiencies. Meanwhile, the Vitamin D Council recommends a UL of 10,000 IUs per day.
In setting its ULs, the IOM considered hypercalcemia as an indicator of vitamin D toxicity. It noted that several studies suggested J- or U-shaped curves of the relationship between vitamin D levels and risk of mortality in which, as vitamin D levels rise, mortality risk falls, until levels reach 75 nmol/L, at which point mortality risk increases.
Hollis rejected the conclusions of these studies and suggested that research, including his own, has shown otherwise. In particular, he cited a study he recently presented as an abstract. This randomized controlled trial of 476 mother-infant dyads looked at whether high daily vitamin D intake by breast-feeding mothers would meet vitamin D needs of both the mother and infants. The researchers found that mothers who received 6,400 IUs per day safely improved their own vitamin D status and achieved infant sufficiency at levels equivalent to that of mothers and infants who each received 400 IUs per day.
"In our studies and others, subjects have been given 2,000–6,000 IUs per day over a period of time, and we've never seen adverse events. This is normal human physiology. We make that much from the sun. Why would you think giving it orally is going to have any different effect? I keep saying they're looking for something that isn't there," Hollis contended.
Hollis's findings aside, studies continue to suggest some limit to vitamin D's protective benefits. For example, in a recent study examining the relationship between vitamin D levels and all-cause and cardiovascular disease-related mortality, Amer found that once 25(OH)D levels rise above 21 ng/mL it offers no statistically significant protection for all-cause mortality. Similarly, Israeli researchers recently reported that vitamin D in the 20–36 ng/mL range was associated with the lowest risk for mortality and morbidity, but that the hazard ratio below and above this range increased significantly.
Manson emphasized that the IOM panel observed "absolutely no rigorous evidence that taking more than the recommended daily allowance of 600 to 800 IU per day conferred greater health benefits, but few randomized trials have tested 2,000 IU per day or higher," she said. "How can we be at a point in 2013 where we're making public health recommendations to take mega-doses of a nutrient that has not been rigorously tested in randomized trials to ensure that the benefits of high doses outweigh the risks?"
Will VITAL Have Answers?
Manson might not have an answer to her question this year, but solid evidence could be on the scene by 2017, thanks to a major randomized controlled trial of which she is the principal investigator. The Vitamin D and Omega-3 Trial (VITAL), a randomized, double-blinded, placebo-controlled, 2x2 factorial trial of a general population of 25,000 U.S. adults, is exploring the relationship between vitamin D and omega-3 fatty acids and risk of cancer and cardiovascular disease. At least 16 ancillary studies are investigating how these agents affect risk of other conditions ranging from cognitive decline and infections to diabetes and lupus. VITAL subjects will receive 2,000 IU/day of vitamin D and 1 g/day omega-3 supplements. In addition to baseline and follow-up blood sample testing, the researchers will genotype a large percentage of participants. Already 24,000 subjects have been recruited, and with a mean treatment period of 5 years. Manson expects to have the first results by 2017.
"We have the advantages of a very large study where we can look at clinical endpoints. With a factorial design, we'll also be able to look at the independent effect of the vitamin D, as well as a possible joint synergistic effect between vitamin D and omega-3 fatty acids," she explained. "We're well aware that no matter what the outcome of the trial, there will be critics who say the dose wasn't high enough, or that it was too high. Or why it did or did not have the expected or hoped for results. However, we feel this is an important opportunity to provide rigorous evidence on whether vitamin D can prevent these major health outcomes."