Until recently, the book on celiac disease (CD) was closed, or so it seemed. Evidence shows that CD, an intestinal inflammatory disease, occurs in genetically susceptible individuals once they are exposed to proteins like gliadin, secalin, and hordein found in wheat and other grains. This model still holds for CD, an autoimmune disorder which historically affected about 1 in 500 people, but is rising in prevalence, at least doubling every 15 years, according to one study. However, a confluence of basic science discoveries and natural history and observational studies is providing a more nuanced picture of CD. Ground-breaking research already has implicated the gut microbiome as a player in turning genetic predisposition and environmental exposure into a full-blown autoimmune response, with further studies underway. This eventually could lead to fundamentally new ways to diagnose and manage CD.
“Our understanding of celiac disease has changed quite dramatically. We were working with some specific paradigms or almost dogmas that we thought would never change,” recalled Alessio Fasano, MD, director of the Mucosal Immunology and Biology Research Center, and of the Center for Celiac Research at Massachusetts General Hospital for Children in Boston.
Settled Science?
One of those paradigms not in dispute is the genetic component of CD. Human leukocyte antigen (HLA) class II genes—DQ2 and DQ8—are present in better than 90% of individuals with the disease. In contrast to other autoimmune disorders, the environmental trigger for CD also is clear: gluten-free diets largely resolve symptoms and restore normal intestinal histology. However, studies and clinical experience have made clear that genetics and the environment are necessary but not alone sufficient to activate CD. For instance, a natural history study Fasano conducted found two patients who did not have positive CD serology until their late 60s (Ann Med 2010;42:530–8).
“The question was, how an individual who is genetically skewed to develop celiac disease is exposed to an indisputable trigger of autoimmunity but is able to tolerate it. What happens to this individual that eventually leads to intolerance and causes celiac disease at any age,” said Fasano.
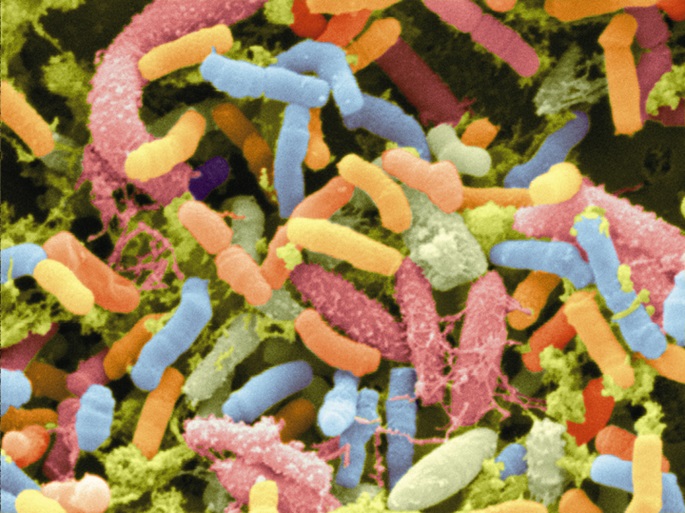
Exploring the Gut Microflora
Interest in a gut microflora role in CD already had begun when, within the past 6 years, the National Institutes of Health Human Microbiome Project as well as next generation sequencing technologies provided data and methods to look more seriously at this issue. That, Fasano’s team and other research groups have begun to do, and their results so far are intriguing.
Fasano and his colleagues in 2012 published a small proof-of-concept study that showed 2-year longitudinal changes in the intestinal microbiota of babies genetically at risk for CD (Plos One 2012;4:e33387). Using pyrosequencing, a quantitative polymerase chain reaction assay, and 1H-nuclear magnetic resonance spectroscopy, the team characterized the gastrointestinal colonization process. They found that genetically susceptible babies first exposed to gluten at age 1 year rather than between 6 to 8 months showed a decreased immune response to gluten. In contrast to other studies, the researchers also reported a dearth of phylum Bacteroidetes in these infants.
This work and other analyses led Fasano to embark on an international study that aims to enroll 500 infants for the purpose of identifying and validating a specific microbiotic and metabolomic profile that predicts loss of tolerance to gluten and development of CD.
Fasano’s, however, is not the only trailblazing effort looking at the microbiomic link to CD. In a series of reports dating back at least 6 years a Spanish team also has been elucidating the connection.
Does Genotype Dictate Microbiota?
Most recently, this group, led by Yolanda Sanz, PhD, reported that HLA-DQ2 genotype per se influences the early gut microbiota composition in infants at risk of developing CD (Gut 2014; doi:10.1136/utjnl-2014-306931). In a subset of a larger prospective study, the researchers found that in comparison to non-HLA-DQ2 babies, HLA-DQ2 babies had higher proportions of phyla Firmicutes and Proteobacteria and lower proportions of Actinobacteria. Sanz’s team in 2013 also showed that infections and antibiotics in the first 4 months of life in infants at risk of CD are the early environmental factors most strongly associated with specific lymphocyte populations and with microbiota composition (Nutr Hosp 2013;28: 464–73).
“According to our data, the microbiome can be influenced by both genetic and environmental factors. These results are associations, so we still have to find out whether these alterations in the microbiome are really related to the development of the disease. We are following up on this now,” said Sanz, a senior researcher at the Institute of Agrochemistry and Food Technology’s Spanish National Research Council, and head of the Research Group on Microbial Ecophysiology and Nutrition at the University of Valencia.
Sanz’s team earlier this year also reported results from a small double-blind, randomized, placebo-controlled trial in which they assessed an exploratory intervention in children newly diagnosed with CD (Br J Nutr 2014;112:30–40). In comparison to those who received placebo, children on a gluten-free diet who daily took Bifidobacterium longum CECT 7347 had reduced levels of potentially pro-inflammatory Bacteroidetes fragilis bacteria, secretory IgA, activated T-lymphocytes, and tumor necrosis factor-X, all of which might “contribute to the recovery of immune homeostasis in CD patients,” according to the authors.
Paving the Way for Personalized Medicine
Although Sanz and Fasano both emphasize that their work is still preliminary, it could have profound implications for the diagnosis and management of CD. Sanz points to three major outcomes of these lines of investigation. “First, to identify biomarkers of the disease. Second, to make stronger recommendations about lifestyle habits that can promote a healthy microbiota at the early stages of life and reduce the risk of the disease,” she explained. “Third would be to design interventions and strategies to minimize the risk of developing celiac disease.”
Fasano thinks the CD-related discoveries ultimately could lead to better diagnostics and treatments for other autoimmune diseases. “These conditions all are very complex, but they’re the final destination. How you get there may change from one individual to another,” he explained. “We make the assumption they are all equal, but it’s not true.” Microbiomic validations along with CD’s clear environmental trigger and comparatively straightforward genetic component lend themselves to a personalized medicine approach, contended Fasano.
This future of a personalized medicine approach writ large for CD and potentially other autoimmune diseases necessarily will involve laboratorians, he added. “The lab would be of monumental importance. We need validated biomarkers that enable the lab folks to say, ‘This individual gets to the final destination through this route, and therefore, needs to be managed this way’,” said Fasano. “These validated tests would all be in the lab, and they would not just be supportive, but instrumental, to decide the therapeutic approach.”
“Our understanding of celiac disease has changed quite dramatically. We were working with some specific paradigms or almost dogmas that we thought would never change.”