 Charles D. Hawker, PhD, MBA, FACB
Charles D. Hawker, PhD, MBA, FACB
Professor (Adjunct) of Pathology,
University of Utah
Scientific Director of Automation and Special Projects
ARUP Laboratories, Salt Lake City
 Bonnie L. Messinger, CMQ/OE (ASQ), CPHQ,
Bonnie L. Messinger, CMQ/OE (ASQ), CPHQ,
Six Sigma Black Belt
Process Improvement Manager
ARUP Laboratories, Salt Lake City
The incidence of patient identification errors, including mislabeled and misidentified specimens, is much too high in clinical laboratories. The best data on errors in U.S. laboratories is derived from three separate College of American Pathologists (CAP) Q-Probe studies, in which the reported rates of mislabeled specimens were 0.39/1000 in 120 institutions (2006), 0.92/1000 in 147 clinical labs (2008), and 1.12% of blood bank specimens in 122 clinical labs (2010). These are sobering statistics, especially for professionals engaged in providing life-sustaining health services. None of us will disagree that the goal for all laboratories is zero misidentified specimens. But how to realize that aim is less clear.
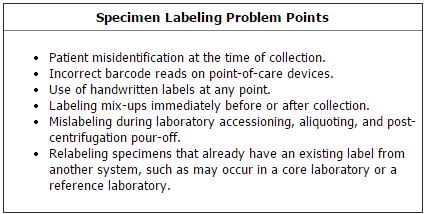
One of the challenges laboratories face is that specimen mislabeling can occur at multiple points in the pre-analytic process (See Box, right). While these single-point weaknesses exist within an infinite set of complex and continually changing processes, a few practical steps can be taken to eliminate these errors. Some of the solutions are easy to implement and others are more costly and involved.
One approach—single piece flow—will be familiar to Lean practitioners. This concept has significant error-proofing potential for labeling tasks at relatively low cost. For example, to prevent errors during collection and processing, avoid having specimens from multiple patients in the active work area at the same time. Also, avoid using strips of labels from a label printer with labels for multiple patients that must be matched to specimens. Unused labels should be destroyed before proceeding to the next patient. Aliquot labels which have limited identifiers and truncated names should be avoided. If aliquoting manually, pour off and label only one specimen at a time before proceeding to the next specimen. Similarly, if using an automated aliquoting device, be sure that the label exactly duplicates the barcode label from the primary tube to facilitate error detection.
Another tool that more laboratories are using is the portable barcode scanner. These scanners read wristband barcodes at point-of-collection and work well in conjunction with portable barcode label printers or point-of-care analytical devices. However, barcode devices make more errors than commonly believed. Snyder et al. made several recommendations to improve the accuracy of barcode reading.
One of the most important actions a laboratory can take to is to implement the CLSI Standard AUTO12-A, Specimen Labels: Content and Location, Fonts, and Label Orientation. Many hospital laboratories have extensive outreach programs or serve as core laboratories for other laboratories and clinics, and most laboratories refer samples to reference labs. This requires sample relabeling, introducing another error-prone step. Often the information systems for these separate facilities differ, and the printed specimen labels have different formats and fonts. Even when specimens are not relabeled, employees must transition quickly and accurately between various fonts, formats, and identifiers. Display and layout inconsistency also leads to an increase in errors. CLSI developed the AUTO12-A standard specifically to deal with the incidence of mislabeled specimens arising from formatting inconsistencies.
Figure 1 (p. 13) shows samples for a fictitious patient using two versions of the label specified by the standard. One version has a vertical zone at the left end of the label which can be used as a reverse font indicator of a priority, such as STAT. The entire top line of each label is reserved for the patient name to limit any possibility of truncation of a long name. The standard, however, does have a very detailed description of a recommended rule for name truncation written in a manner that can be directly implemented in the laboratory information system (LIS) by a software engineer.
Figure 1
Examples of specimen labels that follow the CLSI Standard AUTO12-A.
 Used with permission from the Clinical and Laboratory Standards Institute (CLSI) www.clsi.org.
Used with permission from the Clinical and Laboratory Standards Institute (CLSI) www.clsi.org.
On the second line of the label, left-justified, is the secondary unique identifier used by the institution in compliance with regulatory guidelines. Right-justified on the second line are the patient’s date of birth, age, and sex. Below the barcode, left-justified, are the collection date and time. Alternatively, if the labels are printed prior to specimen collection, that space can be reserved for hand writing the collection date and time with the collector’s ID as required.
Although the standard does not specify fonts for the label, it does recommend the use of a sans serif font, because the serifs—the small tails at the tops and bottoms of characters—make characters harder to read. A minimum font size is specified and spacing is to be adequate so that adjacent characters do not touch each other, either vertically or horizontally. Often laboratories attempt to squeeze as much information as possible on the labels by decreasing font size and crowding the characters and lines closer together, which makes the content more difficult to read.
Under the standard, labels are affixed lengthwise along the tube while holding the tube by its cap or stopper with the left hand. This ensures that the vertical priority zone is on the upper end of the tube when it is held in a rack or an automation carrier so it can be easily viewed. CLSI has received preliminary indications from both CAP and the Joint Commission that the AUTO12-A standard will be referenced in inspection checklists in the coming years. Enforcing this standard will significantly improve laboratory labeling accuracy.
Figure 2
An automated camera system developed for photographing
specimen tube exteriors for vision processing and optical character
recognition analysis to detect possible mislabeled specimens.
Our laboratory has invented one high tech solution that we believe will bring our own error rate for mislabeled specimens to near zero and which, with further refinement, may become suitable for use on commercial automation systems. This is a robotic camera system that can lift a specimen tube from the transport carrier on our automated track, take four simultaneous photographs of the tube using four equidistantly spaced high resolution cameras, precisely stitch the four photographs into a single photograph of the entire exterior of the tube, and then use optical character recognition (OCR) to compare the patient name on the original label to the patient name in our LIS (as identified by reading the barcode on our LIS label). The description and validation of this system has recently been published. Figure 2 is a photograph of the robotic system.
One reason we developed this robotic camera system is that, although the incidence of mislabels from our specimen processing function (approximately 1/8000) is lower than the reported incidences noted above in the CAP Q-Probe studies, our objective of zero mislabeled specimens has remained elusive. We implemented the robotic system in our testing environment in October 2012. Since that time, the system has collected and analyzed some 2.4 million images and more than 300 mislabeled specimens have been detected, of which only 53% were found through our normal quality assurance processes. For the subset of specimens routed through this advanced automation, significantly fewer corrected reports have been issued.
When placed in full production, this technology offers us the prospect of meeting our objective of zero mislabeled specimens escaping the pre-analytical process, at least for that portion of our laboratory’s work that passes through the OCR analysis. As we gain more experience with this technology, we anticipate that it can be widely used, especially in higher volume settings.
FURTHER READING
- Bonini P, Plebani M, Ceriotti F, et al. Errors in laboratory medicine. Clin Chem 2002;48:691–8.
- Clinical and Laboratory Standards Institute (CLSI). Specimen labels: Content and location, fonts, and label orientation; approved standard. CLSI document AUTO12-A. Wayne, Pa.: CLSI 2011.
- Grimm E, Friedberg RC, Wilkinson DS, et al. Blood bank safety practices: Mislabeled samples and wrong blood in tube – a Q-Probes analysis of 122 clinical laboratories. Arch Pathol Lab Med 2010;134:1108–15.
- Hawker CD. Bar codes may have poorer error rates than commonly believed. Clin Chem 2010;56:1513–4.
- Hawker CD, McCarthy W, Cleveland D, et al. Invention and validation of an automated camera system that uses optical character recognition to identify patient name mislabeled samples. Clin Chem 2014;60:463–70.
- Snyder ML, Carter A, Jenkins K, et al. Patient misidentifications caused by errors in standard bar code technology. Clin Chem 2010;56:1554–60.
- Valenstein PN, Raab SS, Walsh MK. Identification errors involving clinical laboratories: A College of American Pathologists Q-Probes study of patient and specimen identification errors at 120 institutions. Arch Pathol Lab Med 2006;130:1106–13.
- Wagar EA, Stankovic AK, Raab S, et al. Specimen labeling errors: A Q-Probes analysis of 147 clinical laboratories. Arch Pathol Lab Med 2008;132:1617–22.